Some Common Complications during Pregnancy
Bleeding
Although frequent throughout pregnancy, bleeding can sometimes indicate premature labor, vaginal or cervical infection, or issues related to the placenta. Late-stage pregnancy bleeding may increase the chance of major problems and may need medical intervention, including an early delivery. Any bleeding that occurs during pregnancy has to be reported to your doctor right away.
Complications with Amniotic Fluid
The liquid in the sac around the fetus is called amniotic fluid, and an excessive amount or shortage of it might indicate a pregnancy issue. An excess of fluid can cause problems like the mother breathing becoming worse and premature labor or early rupture of the membranes.
Diabetes, multiple pregnancies (twins or triplets), infections, incompatible blood types, and birth abnormalities are common reasons of excessive fluid intake. Along with placental issues, slower fetal growth, premature membrane rupture, and fetal mortality, low fluid levels can also indicate birth abnormalities.
Amniotic fluid protects a fetus from harm by cushioning the womb. It also aids in regulating the wombs internal temperature. Certain natural activities of the womb are disrupted by either an excessive amount of amniotic fluid (polyhydramnios) or an insufficient amount (oligohydramnios).
A baby ability to correctly grow their muscles, limbs, lungs, and digestive system might be hampered by low amniotic fluid.
Miscarriage
A miscarriage occurs when a pregnancy ends before the full 20 weeks. 10 to 20 percent of pregnancies result in miscarriage. In the first trimester, miscarriages account for more than 80% of cases. Severe cramps and bleeding are common before miscarriages. The doctor may prescribe blood tests and an ultrasound to confirm a miscarriage. A dilation and curettage operation, which utilizes specialized equipment to remove the defective pregnancy, can be needed if the fetus and contents of the uterus do not spontaneously discharge. If this does not happen, medication can be used to induce it.
Hyperemesis gravidarum
Although nausea and vomiting are typical throughout the first trimester of pregnancy, excessive and prolonged nausea and vomiting, or hyperemesis gravidarum, can cause dehydration and weight loss. Medical intervention may be necessary to treat this illness.
Ectopic Pregnancy
An ectopic pregnancy occurs when a fertilized egg is placed outside of the uterus. Usually, one of the fallopian tubes is where the egg rests. A fetus cannot develop normally there due to space constraints and a shortage of supportive tissues. An ectopic pregnancy is potentially fatal and can result in excruciating agony and harm to a woman’s reproductive system. The fallopian tube may break as the fetus grows, resulting in serious internal bleeding (hemorrhage).
Ectopic pregnancies account for roughly 2% of all pregnancies, and about half of these cases have no recognized cause or risk factors.
Gestational Diabetes
Gestational diabetes is a condition in which the body either produces insufficient insulin or uses it improperly due to hormonal changes brought on by pregnancy. Instead, diabetes, sometimes referred to as high blood sugar, is brought on by an accumulation of glucose in the blood.
Controlling gestational diabetes by adherence to a physician prescribed treatment plan is the most effective means of mitigating or averting complications linked to elevated blood sugar levels during pregnancy.
Thyroid Problems
Pregnancy may be impacted by thyroid conditions such as hyperthyroidism or hypothyroidism. The development of the baby brain and nervous system depends on the thyroid gland functioning properly.
Congenital Disorders
You have a higher chance of experiencing pregnancy difficulties if your healthcare professional believes the fetus has a congenital ailment or health concern. This might indicate that you require closer supervision or that your newborn requires particular attention.
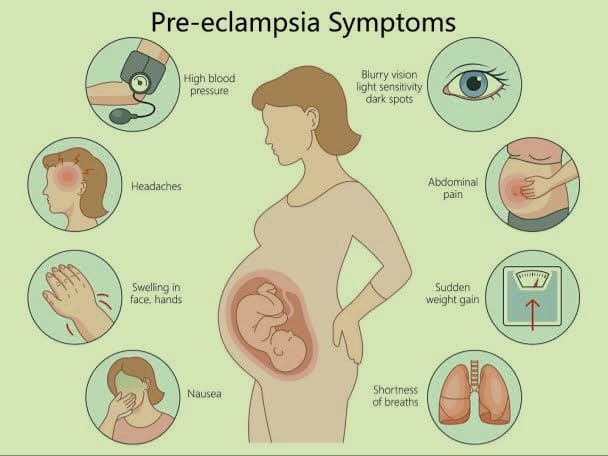
Preeclampsia
Elevated blood pressure and elevated protein levels in a woman urine are symptoms of preeclampsia. Usually after the 20th week of pregnancy, preeclampsia develops. It’s a dangerous illness that can cause premature birth and even death.
Eclampsia
Eclampsia is a condition in which seizures are brought on by the central nervous system being attacked by preeclampsia. It’s a really dangerous illness. It can be deadly for the mother as well as the child if left untreated. It is extremely uncommon for the more controllable preeclampsia to develop into eclampsia, nevertheless, when appropriate prenatal care is provided.
Infections
During pregnancy and or delivery, infections, including some STIs, can arise. These infections can cause issues for the pregnant woman, the pregnancy, and the infant following delivery. Certain illnesses can spread from mother to child through the birth canal during childbirth, while other infections can infect a developing fetus throughout pregnancy.
Molar Pregnancy
A placental anomaly is known as a molar pregnancy. It occurs when, following fertilization, an aberrant mass develops inside the uterus rather than a typical embryo. Molar pregnancies, also known as gestational trophoblastic illness, are uncommon.
Molar pregnancies come in two varieties: Complete and Partial. The fertilization of an empty egg by the sperm results in complete molar pregnancies. There is no fetus within, but the placenta develops and releases the pregnancy hormone. When a mass emerges that includes both the aberrant cells and an embryo with severe abnormalities, it is known as a partial molar pregnancy. In this instance, the expanding aberrant bulk would soon overwhelm the fetus.
Preterm labor
When labor begins before 37 weeks of pregnancy, it is referred to as preterm (early) labor. This might result in your baby being born underweight or with undeveloped organs.
What Are Things That Are Not Normal During First Trimester?
Pregnancy causes a variety of painful symptoms, some of which are brought on by hormonal changes. Others might be linked to your developing baby weight and pressure.
Excessive Bleeding: Light spotting may be typical, but severe bleeding—especially in the case of clots—may indicate a miscarriage or other problems.
Severe abdominal pain: While mild cramping is typical as the uterus grows, severe or ongoing discomfort in the abdomen may be a sign of an ectopic pregnancy or miscarriage.
Hyperemesis gravidarum, or extreme nausea and vomiting: Although morning sickness is normal, severe and prolonged vomiting can cause dehydration and necessitate medical intervention.
Severe headaches or visual disturbances: Prolonged, intense headaches or vision abnormalities may indicate the presence of preeclampsia or other disorders.
Fever and illness: If a pregnant fever is present together with other symptoms, it may be a sign of an infection that might be dangerous to the growing fetus. Such as dizziness, intense nausea or vomiting, or a temperature that is higher than usual.
Pelvic pain or pressure: If pelvic pain or pressure persists, it may indicate a problem, such as an ectopic pregnancy or a threatening miscarriage.
Issues with Urination: This refers to burning or agony during urinating, particularly if a temperature is present.
Absence of fetal movement: Although fetal movement is typically not felt until much later in pregnancy, it may be cause for concern if it is observed on an ultrasound or other test.
Risk Of Miscarriage During First Trimester
Pregnancy before to week 20. Within the first 12 weeks of pregnancy, or the first trimester, is when most miscarriages happen. Numerous variables might impact the likelihood of miscarriage, and it’s crucial to remember that genetic disorders are a common cause of miscarriages that are out of anyone control.
Chromosome Issues
They include a comprehensive collection of instructions that regulate many different aspects of life, including as the color of a baby eyes to the way body cells grow. There are situations where an error occurs during conception, resulting in an excess or deficiency of chromosomes in the developing embryo. This indicates that the baby won’t be able to develop correctly, which will lead to a miscarriage, however the exact causes are frequently unknown.
Your Age
According to studies, the risk of miscarriage increases from 12% to 15% in one 20s to around 25% by the time one reaches 40. The majority of miscarriages associated to ageing result from chromosomal abnormalities, when the fetus has an excess or missing chromosome.
Health Conditions
You have a higher risk of miscarriage if you have certain health disorders such uncontrolled diabetes, infections, or problems with your uterus or cervix. Consult your prenatal care physician about miscarriage risk factors. Once they’ve looked over your medical history, they may talk about your risk.
Miscarriage risk can be impacted by a number of maternal health concerns, including diabetes, thyroid issues, and autoimmune illnesses. For example, poorly managed diabetes may raise the risk.
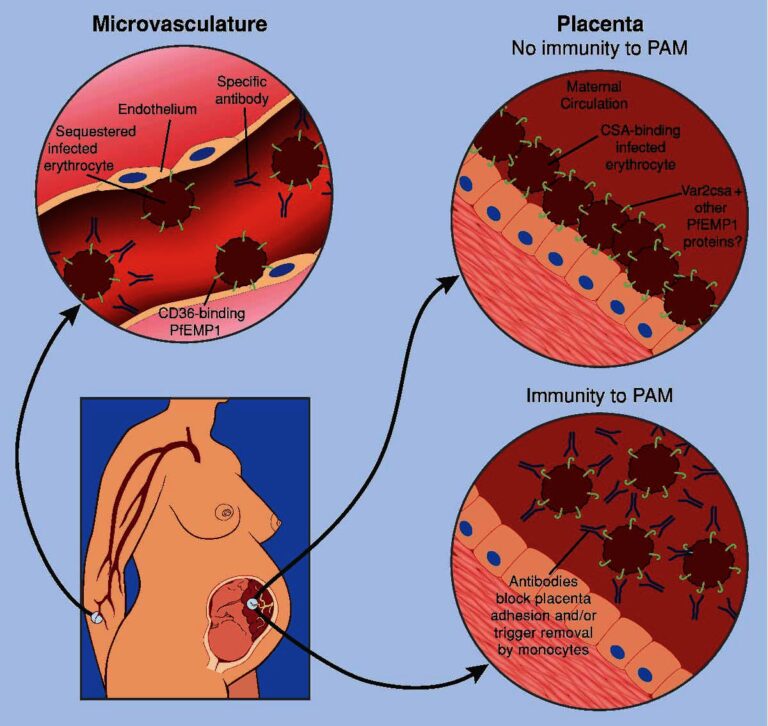
Placenta Problems
The organ that connects your blood supply to your baby called the placenta. An issue pertaining to placenta development may potentially result in miscarriage.
Previous miscarriage
If you have previously experienced a miscarriage, your chances of having another one is 25%, which is just slightly greater than those of someone who has never experienced one.
Hormonal Imbalances
The growth and maintenance of the uterine lining as well as the embryo can be impacted by hormonal imbalances, particularly those involving progesterone.