Micronutrients and Pregnancy
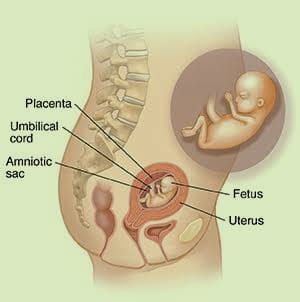
The state of pregnancy is defined as a period of enhanced metabolic demand. Due to changes in a woman’s physiology and the demands of fetal growth. During this period, insufficient stores or micronutrient consumption may be negative Implications for the mother such as anemia, hypertension, various labor complications, and death. It can also affect the fetus, resulting in stillbirth, premature delivery, intrauterine growth retardation, birth defects, immunodeficiency, and organ abnormalities. Developmental deficiency of these nutrients can lead to maternal morbidity and mortality. Because they are important for fetal development.
Causes of Micronutrient Deficiency
Inadequate intake or poor absorption, which can result from diseases or persistent inflammation, can both lead to micronutrient deficiencies. Micronutrient deficiency in children can be attributed to either rapid postnatal growth or maternal micronutrient deficiency during pregnancy.
Important of Micronutrients in Pregnancy
The metabolic needs of pregnant women are significantly higher, leading to increased micronutrient levels to meet the body’s nutritional needs.
- Zinc
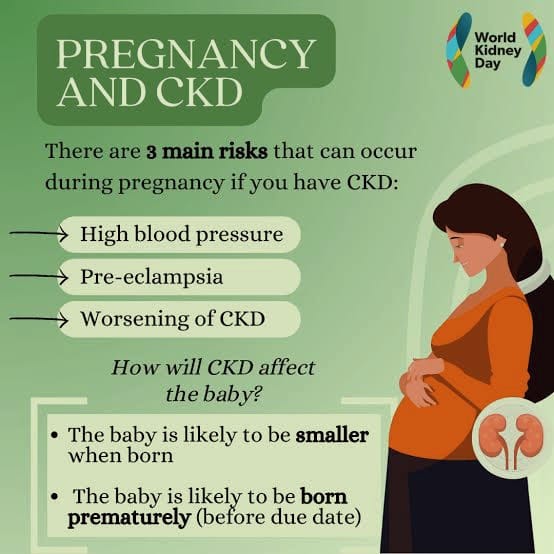
According to studies conducted on expectant mothers, severe zinc deficiency can significantly affect pregnancy outcomes. Preeclampsia, premature rupture of membranes, cleft lip, preterm birth with impaired fetal growth, and congenital abnormalities are among the pregnancy problems and birth outcomes that are associated with it. Severe zinc deficiency results in teratogenesis, ongoing labor, and fetal or fetal death. Fetal immune system development is adversely affected by zinc deficiency in utero in several ways. Pregnant women who take zinc supplements benefit their unborn babies by having stronger immune systems, less diarrhea and fewer respiratory illnesses. Zinc intake during pregnancy should not exceed 12 mg. Meat, fish, oysters, whole grains, eggs, nuts and other foods are good sources of zinc.
- Iron
During pregnancy, iron is one of the main trace metals that are needed. Preterm birth and maternal anemia have been linked to iron deficiency during pregnancy. From the moment of conception, during the pregnancy, and during nursing, enough iron is needed. Mental impairment during breastfeeding may be linked to iron deficiency. For women who are pregnant, a daily iron intake of 27 mg is advised. Liver, beef, fortified cereals, cashew nuts, and baked beans are foods that are good dietary sources of iron (i.e., more than 2 mg/serve). It is thought that having too much iron might prevent other vitamins from being absorbed, however this theory has not yet been thoroughly proven.
- Folic Acid
Folic acid is traditionally given in combination with folic acid as a supplement during pregnancy mainly because of its benefits for hematopoiesis. Despite the fact that deficiencies have also been linked to birth abnormalities and difficulties during pregnancy. There is uncertainty about the involvement of folic acid deficiency in various birth outcomes, including low birth weight, preterm birth, and perinatal death. According to the limited evidence available, pregnant women in underdeveloped countries may benefit from folic acid supplementation in terms of improved fetal growth and reduced risk of low-birth-weight babies.
- Iodine
Iodine is essential for the growth and development of fetuses and infants. Stillbirth or stillbirth, fetal abnormalities, neurologic cretinism, or mental retardation with deafness, spastic diplegia, squint, and myxoedematous cretinism are all possible consequences of severe iodine deficiency. Pregnant women should drink at least 220 µg per day.
- Phosphorus
Phosphorus is known to activate catalytic proteins and regulate blood acid-base balance in the form of phosphate. Although rare, deficiency of this mineral can cause symptoms including rickets, anorexia, ataxia, paralysis, anemia, muscle weakness, and even death. There is no dietary phosphorus deficiency, and pregnant women should consume approximately the same amount as non-pregnant women.
- Sodium
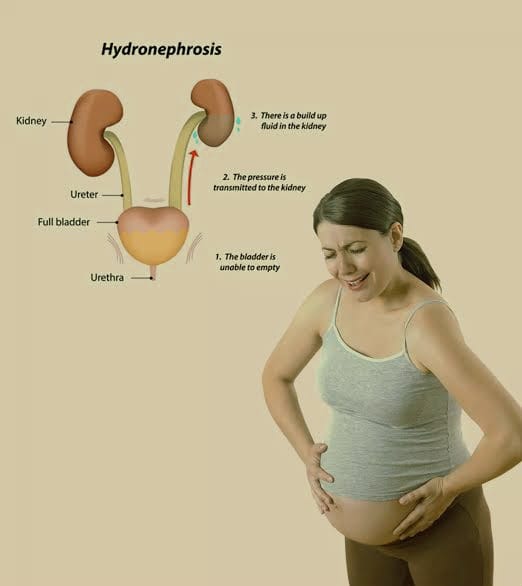
Natural nutrients like sodium are essential for various body processes. Sodium helps in fetal development by maintaining pH balance and fluid levels. The Recommended Daily Allowance (RDA) for salt for pregnant women is 3.8 grams. In the absence of salt, nerves, muscles and organs do not function properly. On the other hand, high consumption of salt during pregnancy increases the risk of high blood pressure, cardiovascular diseases, etc.
- Vitamins
Vitamins are an organic molecule that is essential to the metabolism of different pregnant people to function properly. There are two types of them: soluble in fat and soluble in water.
- Vitamin A
Vitamin A deficiency is associated with preterm birth, low birth weight, placental abruption, increased maternal mortality, and intrauterine development retardation. Additionally, studies have shown that in a population of mothers with mild to moderate hemoglobin levels, vitamin A supplementation can increase hemoglobin concentrations by approximately 4 g/L. 800 µg per day is recommended for pregnant women. An excellent source of vitamin A is breast milk. On the other hand, adequate amounts of vitamin A in breast milk are essential for adequate nutrition in mothers.
Orange and yellow vegetables (carrots, sweet potatoes, pumpkins, and other winter and summer squashes), as well as leafy greens (kale, spinach, broccoli), Tater, Black pepper in red, Mango with Cantaloupe, fish oil; Liver of cattle, Eggs from milk, Fortified foods.
- Folate
It is very important for fetal development. It is an essential factor in the synthesis of nucleotides and the conversion of homocysteine to methionine, which is used in the methylation of proteins, lipids, and DNA. Folate deficiency is associated with an increased risk of congenital abnormalities, low birth weight, preterm delivery, and preeclampsia. The Recommended Daily Allowance (RDA) of folate for pregnant women is 600 micrograms. High folate foods include leafy green vegetables, legumes, and other foods.
- Vitamin D
Vitamin D is a class of fat-soluble prohormones that aid in the absorption of calcium and phosphorus from food, both of which are essential for fetal skeletal development. An unborn baby with type 1 diabetes mellitus or rickets can be the result of vitamin D deficiency during pregnancy. During pregnancy and breastfeeding, a daily intake of 5 µg of vitamin D is recommended. On the other hand, overuse of supplements may be harmful as it is associated with fatigue and loss of appetite in mothers.
Dairy products and grains are among the many foods and supplements that have been fortified with vitamin D. Salmon, swordfish, tuna, cod liver oil, and vitamin D-fortified orange juice. Plant-based and dairy milks are fortified with vitamin D. Egg yolks, beef liver, sardines, and fortified cereals.
- Vitamin C
Vitamin C promotes better absorption of iron, which reduces the incidence of maternal anemia. It also protects the body from harmful free radicals as an oxidant. Vitamin C deficiency alone has not been shown to cause difficult labor, although it is thought to be a contributing factor. During pregnancy, 60 mg of vitamin C per day is recommended.
Oranges and their juice, peppers, strawberries, blackcurrants, broccoli, Brussels sprouts, potatoes and other citrus fruits are good sources.
- Vitamin E
In the lipid phase of the cell membrane, vitamin E acts as an antioxidant by preventing free radical damage to polyunsaturated fatty acids. Increased consumption of vitamin E has been linked to a lower risk of heart disease, diabetes problems, some types of cancer and cataracts. When a woman is pregnant, the recommended daily intake is equal to her normal daily requirement (7 mg/day), but increases to 11 mg/day while breastfeeding.
Vitamin E includes cooking oils (safflower, sunflower, and wheat germ oils). Nuts and seeds, including peanuts, hazelnuts, almonds, and peanut butter. Fish (salmon, trout and abalone). Vegetables (butternut squash, turnip greens, and red bell peppers). Fruits (kiwi fruit, avocados, and mangoes).
- Vitamin K
Vitamin K (VK) deficiency can be especially dangerous for pregnant mothers and babies, as it can cause hemorrhage. Prothrombin required for blood clotting is VK. As a result, when prothrombin levels fall, blood clotting also slows, which can lead to heavy bleeding in the mother or newborn.
Foods high in vitamin K are fresh, raw salads and leafy greens such as broccoli and spinach.
Celery, leeks, artichokes, beans, peas, and red cabbage Dairy products such as milk, cream, and cottage cheese, rapeseed and olive oil Lean meats that are well-cooked.