Pregnancy and cancer treatment
Introduction
The diagnosis of cancer during pregnancy presents a profoundly challenging scenario, bringing to the forefront a myriad of complexities that intertwine the lives of both mother and unborn child. This delicate situation demands an intricate balance between two equally paramount objectives: preserving the health and well-being of the mother while ensuring the utmost safety and developmental integrity of the fetus. The intersection of pregnancy and cancer diagnosis not only amplifies the emotional and psychological burden on the expectant mother but also complicates the medical approach to treatment, necessitating a careful, nuanced strategy that respects the dual focus of safeguarding maternal health and fetal welfare.
Understanding the Intersection of Pregnancy and Cancer
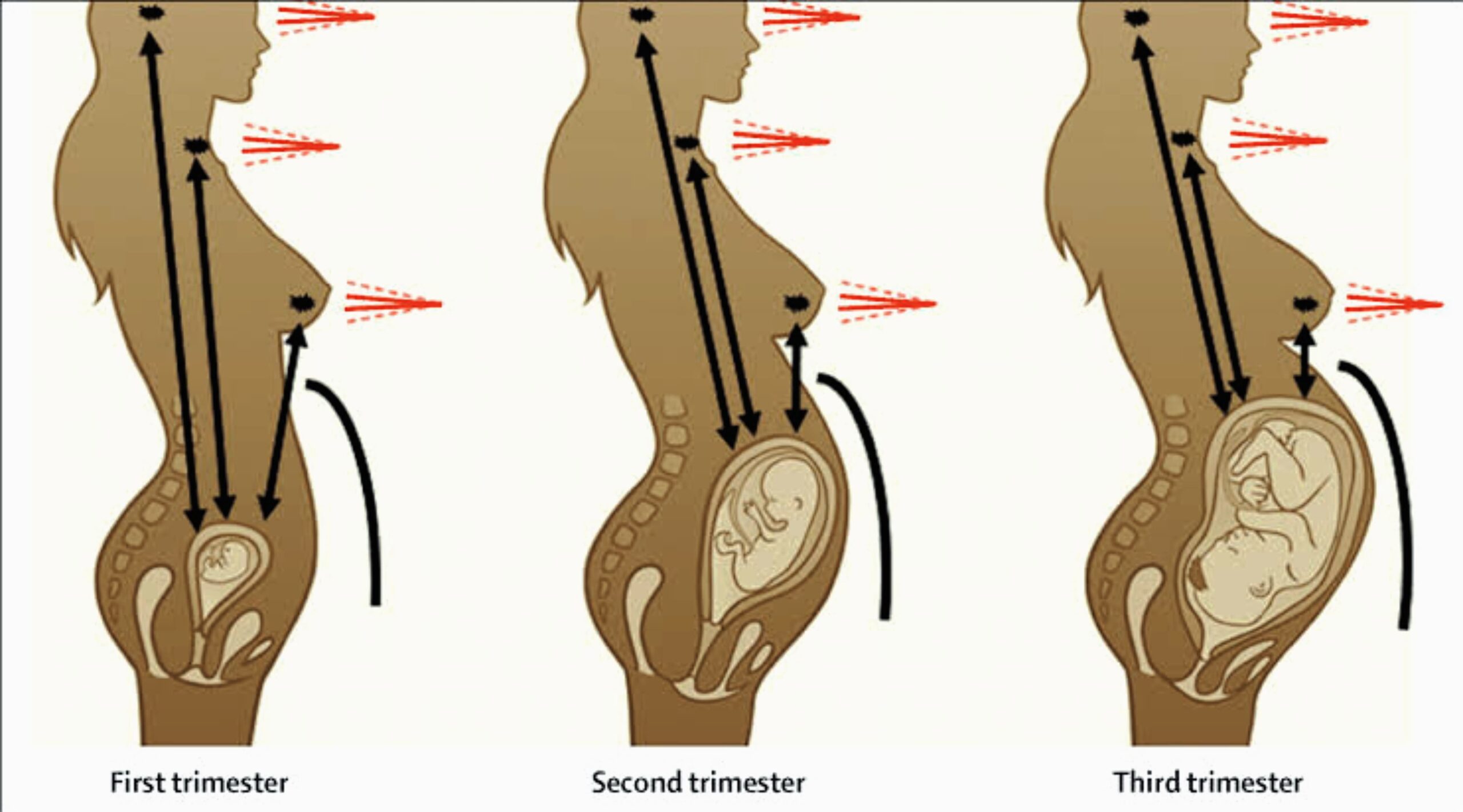
Cancer treatment during pregnancy is a complex interplay of timing, type of cancer, and the specific treatments available, each carrying potential risks and benefits for both the mother and her developing baby. Pregnancy introduces a dynamic physiological state that can significantly affect how cancer is treated. For instance, increased blood flow and changes in the body’s immune system and hormone levels can influence the behavior of cancer cells and the body’s response to treatment. Furthermore, the need to protect the fetus often limits the use of diagnostic imaging and certain treatments, thereby necessitating adaptations to standard cancer care protocols.
The types of cancer most commonly diagnosed during pregnancy include breast cancer, cervical cancer, ovarian cancer, and leukemia. Each of these cancers requires a tailored approach to diagnosis and treatment, taking into account the stage of pregnancy and the specific characteristics of the cancer. For example, breast cancer, the most frequently diagnosed cancer during pregnancy, requires careful consideration of surgical options and the timing of chemotherapy to minimize risks to the fetus. Similarly, the management of cervical and ovarian cancers during pregnancy may involve a combination of close monitoring and delayed treatment until after delivery, if possible, or the consideration of treatments that are deemed safe during certain trimesters.
This introduction sets the stage for a comprehensive exploration of the challenges and considerations inherent in managing cancer during pregnancy. It underscores the critical importance of a multidisciplinary approach that involves oncologists, obstetricians, and pediatricians working in concert to devise and implement a treatment plan that optimally balances the health needs of the mother with the safety of the unborn child.
Diagnostic Challenges
Diagnosing cancer during pregnancy presents a unique set of challenges that complicate both the detection and management of the disease. The symptoms of pregnancy, such as fatigue, nausea, and changes in breast tissue, can closely mimic or obscure the signs of cancer, leading to potential delays in diagnosis. Moreover, the physiological changes that accompany pregnancy can alter the presentation and progression of cancer, further complicating the diagnostic process.
Overlapping Symptoms and Limitations of Diagnostic Tests
The overlapping symptoms between pregnancy and cancer can make it difficult for healthcare providers to immediately suspect and accurately diagnose cancer. For instance, breast changes are common during pregnancy, which can mask symptoms of breast cancer. Similarly, cervical changes and bleeding, which might otherwise prompt investigations for cervical cancer, can be mistakenly attributed to pregnancy-related changes.
The limitations of diagnostic tests during pregnancy pose additional hurdles. Many standard diagnostic procedures, such as certain imaging tests and biopsies, carry risks to the fetus and may need modification or delay. Healthcare providers must balance the need for accurate cancer diagnosis with the imperative to minimize fetal exposure to potentially harmful procedures.
Safe Diagnostic Tools during Pregnancy
Despite these challenges, there are safe diagnostic tools and strategies that can be employed during pregnancy:
Ultrasound: Ultrasound is a primary diagnostic tool that can be safely used during pregnancy for the detection of masses or anomalies in organs like the breast and ovaries.
Magnetic Resonance Imaging (MRI): MRI, without the use of contrast agents, is considered safe during pregnancy and can be valuable for diagnosing and staging certain cancers without exposing the fetus to ionizing radiation.
Biopsy: When a suspicious mass is identified, a biopsy can often be performed safely during pregnancy to obtain a definitive cancer diagnosis. The method and timing of the biopsy are carefully considered to minimize risks.
Healthcare providers often employ a multidisciplinary approach, involving obstetricians, radiologists, and oncologists, to ensure that diagnostic procedures are both safe for the fetus and effective in identifying cancer. This collaborative effort is crucial in navigating the diagnostic challenges and ensuring the best possible outcomes for both the mother and the unborn child.
Treatment Modalities and Their Implications
Treating cancer during pregnancy is a delicate balance between aggressive management of the disease and the preservation of fetal health. The approach is highly individualized, taking into account the type of cancer, its stage, and the trimester of pregnancy. This section explores the various treatment modalities available for pregnant cancer patients, along with the considerations that guide the timing and type of treatment.
Overview of Treatment Options
Surgery: Often considered the safest cancer treatment during pregnancy, especially in the second trimester, surgery poses the least risk to the fetus. The decision to proceed with surgery depends on the cancer type, its location, and the gestational age.
Chemotherapy: Certain chemotherapeutic agents can be administered during the second and third trimesters with relative safety, as the risk of congenital abnormalities is reduced. However, chemotherapy is generally avoided during the first trimester due to the increased risk of fetal malformations.
Radiation Therapy: While radiation therapy is less commonly recommended during pregnancy due to potential risks to the fetus, including growth restriction and malformations, modern techniques can minimize exposure. The decision to use radiation therapy is based on a careful assessment of the benefits to the mother and potential risks to the developing fetus.
Considerations for Timing and Type of Treatment
Cancer Type and Stage: The nature and aggressiveness of the cancer play crucial roles in determining the treatment plan. Early-stage cancers may allow for a delay in treatment until after delivery, while more aggressive types may necessitate immediate intervention.
Pregnancy Trimester: The stage of pregnancy is a critical factor in treatment planning. Treatments posing higher risks to the fetus are more likely to be postponed until the second or third trimester, when fetal organs have developed and the risks of adverse outcomes are lower.
Balancing Maternal and Fetal Health: The overarching goal is to optimize the health outcomes for both the mother and the fetus. This involves a collaborative approach among specialists in oncology, obstetrics, and pediatrics to devise a treatment plan that addresses the cancer effectively while minimizing harm to the fetus.
This intricate process underscores the complexity of cancer treatment during pregnancy, requiring a nuanced understanding of the interactions between cancer therapies and fetal development. The safety and efficacy of each treatment modality are weighed carefully against the backdrop of maternal and fetal health, aiming for the best possible outcomes for both.
Surgery during Pregnancy
Surgery during pregnancy, while complex, is often a feasible option for treating cancer in pregnant patients. The decision to proceed with surgical intervention hinges on a careful evaluation of several factors, ensuring the safety and well-being of both the mother and the fetus.
Feasibility of Surgical Interventions: Surgery is considered relatively safe during the second trimester of pregnancy. This period is often preferred for surgical interventions as the risk of miscarriage is lower compared to the first trimester, and the risk of preterm labor is less than in the third trimester.
Factors Influencing the Timing of Surgery: The timing of surgery during pregnancy is influenced by the type of cancer, its progression, the gestational age of the fetus, and the urgency of treatment. The aim is to balance the need for immediate cancer treatment against the potential risks to the fetus.
Potential Risks to the Fetus: While surgery during pregnancy is generally safe, potential risks include preterm labor and fetal distress, especially if the surgery involves the abdomen or pelvis. Modern surgical techniques and careful monitoring minimize these risks, making it a viable option for many pregnant cancer patients.
Chemotherapy in the Context of Pregnancy
Chemotherapy during pregnancy requires a nuanced approach, balancing the treatment of cancer with the safety of the developing fetus. Guidelines have evolved to ensure that chemotherapy is administered in a manner that considers the unique circumstances of pregnancy.
Guidelines for Administering Chemotherapy: Chemotherapy is generally considered safe during the second and third trimesters, as the risk of congenital abnormalities is significantly reduced. The first trimester is a critical period for fetal organ development, and exposure to chemotherapy during this time is associated with a higher risk of fetal malformations and complications.
Safety of Use During the Second and Third Trimesters: Specific chemotherapeutic agents have been identified as safer for use during the latter stages of pregnancy. These drugs are selected based on their lower risk profiles and the body of evidence supporting their use in pregnant cancer patients.
Potential Risks and Long-term Effects on the Child: While chemotherapy during the second and third trimesters is generally safe, there is ongoing research into the potential long-term effects on children exposed to chemotherapy in utero. These may include issues related to growth, development, and fertility. However, the majority of studies have shown that children born to mothers who received chemotherapy during pregnancy develop normally.
The administration of chemotherapy during pregnancy underscores the importance of a multidisciplinary approach, involving oncologists, obstetricians, and pediatricians, to ensure that treatment decisions are made with the utmost care for both the mother and the fetus.
Radiation Therapy: Risks and Limitations
Radiation therapy during pregnancy is approached with caution due to the significant risks it poses to the developing fetus. These risks include potential birth defects, growth retardation, and an increased risk of childhood cancers. The decision to use radiation therapy is heavily influenced by the type of cancer, its location, the stage of pregnancy, and the urgency of treatment.
Minimizing Fetal Exposure: When radiation therapy is deemed necessary, various techniques and shielding methods are employed to minimize fetal exposure. This might include using lead shields or adjusting radiation beams to limit the dose received by the fetus.
Alternative Treatment Strategies: In many cases, healthcare providers may explore alternative treatment options that pose less risk to the fetus. This could involve delaying radiation therapy until after birth or opting for surgery or chemotherapy if these are considered safer and effective alternatives.
Psychological and Emotional Support Needs
The diagnosis of cancer during pregnancy can be an overwhelming experience, placing immense psychological and emotional strain on the expectant mother. The fear for one’s own life coupled with concerns for the unborn child’s health can lead to significant stress, anxiety, and depression.
Importance of Support: Providing robust psychological and emotional support is crucial. This includes counseling services, support groups, and holistic care approaches that address the mental and emotional wellbeing of the pregnant patient.
Resources and Strategies for Support: Healthcare teams should ensure that pregnant women diagnosed with cancer have access to a range of support services. This could include referral to a psychologist specializing in oncology, access to peer support groups, and the provision of comprehensive information about the diagnosis and treatment options. Family involvement and social support networks also play a vital role in providing emotional stability and practical assistance during this challenging time.
The integration of medical treatment with psychological and emotional support creates a holistic care approach that not only aims to treat the cancer but also supports the patient’s overall wellbeing, ensuring that both mother and baby have the best possible outcomes.