Female Contraception
Downsides of Different female Contraceptive
Introduction
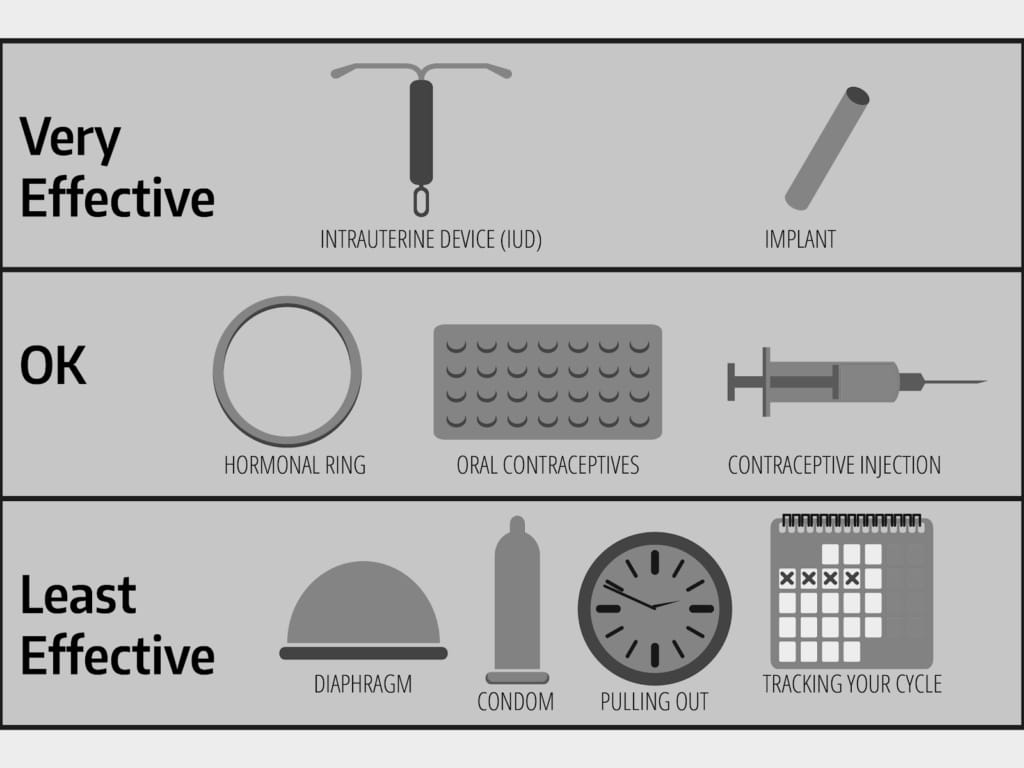
The landscape of female contraceptives is diverse, offering a plethora of choices to suit the varied needs and circumstances of women globally. From hormonal pills to intrauterine devices, each method provides the power to control fertility and make informed decisions about family planning. However, with this empowerment comes the responsibility to understand not only the benefits but also the potential downsides of these contraceptive options.
While contraceptives are celebrated for their role in allowing women to plan if and when they have children, it’s equally important to acknowledge the complexities they may introduce to a woman’s health and well-being. Side effects, ranging from minor inconveniences to more serious health risks, are considerations that women must weigh when selecting the most appropriate form of birth control.
In this discussion, we will delve into the various forms of female contraception, shedding light on the less discussed but equally critical aspect of their use: the downsides. By exploring the potential drawbacks, we aim to provide a holistic view that can guide women in making choices that align with their health priorities, lifestyle, and personal comfort.
Recognizing the potential challenges associated with contraceptive methods is not meant to discourage their use but to promote a deeper understanding and encourage dialogue between women and healthcare providers. This balanced perspective is key to navigating the complex yet vital world of female contraceptives.
Hormonal Contraceptives: Pills, Patches, and Injections
Hormonal contraceptives are a cornerstone of modern family planning, offering effective control over reproductive health. However, they come with a spectrum of side effects that can affect women’s physical and emotional well-being, and there are concerns about their long-term use and the period after discontinuation.
Common Side Effects
Mood Changes: Many women report mood swings and emotional disturbances, which can range from mild irritability to significant depression or anxiety.
Weight Gain: Hormonal contraceptives can lead to weight gain due to changes in appetite, fluid retention, and alterations in body composition.
Health Risks: There are potential long-term health risks, such as increased chances of blood clots, especially in smokers or women with certain health conditions. There’s also a nuanced association with the risk of certain cancers, which varies depending on the type of contraceptive and individual health factors.
Impact on Menstrual Cycles and Fertility
Menstrual Irregularities: Hormonal contraceptives can cause changes in menstrual bleeding patterns, ranging from lighter periods to amenorrhea (the absence of menstruation).
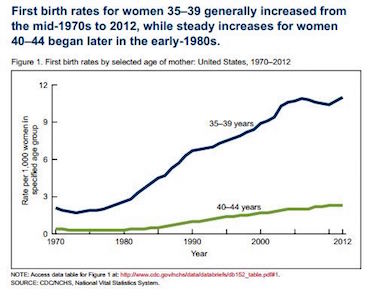
Post-Discontinuation Fertility: There is often concern about how quickly fertility returns after stopping hormonal contraceptives. While most women return to their typical menstrual cycle within a few months, for some, it may take longer to regain fertility.
These potential downsides necessitate that women receive comprehensive counseling before starting hormonal contraceptives. They should be informed about the side effects, how to manage them, and what to expect when they choose to stop using the method. Open discussions about these issues can help women make choices that are right for their bodies and their future family planning goals.
Intrauterine Devices (IUDs): Hormonal and Copper
Intrauterine devices (IUDs), both hormonal and copper, are highly effective long-term contraceptive options favored by many women. Despite their efficacy, they come with specific risks and side effects that can affect a woman’s decision to use them.
Physical Risks of IUDs
Perforation and Displacement: On rare occasions, the insertion process can lead to uterine perforation, or the IUD can become dislodged and move from its proper place in the uterus, potentially causing pain or injury.
Menstrual Changes: Copper IUDs, in particular, may cause increased menstrual bleeding and more severe cramps, which can be distressing and uncomfortable for many users.
Potential Health Complications
Pelvic Inflammatory Disease (PID): Although it’s uncommon, there’s a risk of developing PID, especially shortly after insertion. It’s crucial for potential IUD users to be aware of this risk and the symptoms to watch for.
Hormonal IUD Side Effects: Hormonal IUDs can lead to systemic side effects similar to other hormonal contraceptives, including hormonal imbalances, mood fluctuations, and acne.
Considerations for IUD Users
Informed Consent: Women considering an IUD must be given comprehensive information about these risks and how to identify potential complications.
Regular Checkups: After insertion, regular checkups are necessary to ensure the IUD remains in place and isn’t causing adverse effects.
Intrauterine devices offer a form of contraception that, while effective, requires consideration of the potential physical risks and side effects. Proper counseling, careful insertion, and ongoing medical follow-up are essential components of the IUD experience, ensuring safety and comfort for the user.
Barrier Methods: Diaphragms and Condoms
Barrier methods of contraception, such as diaphragms and condoms, are non-hormonal options that many women and couples choose for preventing pregnancy. While they offer certain advantages, including fewer systemic side effects, they also come with drawbacks that can affect their overall convenience and effectiveness.
Challenges with Barrier Methods
Timely Application: Both diaphragms and condoms require timely, correct application to be effective. This need for immediate and proper use before each sexual encounter can be seen as inconvenient or disruptive to spontaneity.
Risk of Slippage or Breakage: Condoms in particular carry a risk of slippage or breakage during intercourse, which not only compromises their effectiveness but also interrupts intimacy and may cause stress or concern.
Consistency of Use: The effectiveness of barrier methods is highly dependent on consistent and correct use. Unlike long-acting reversible contraceptives (LARCs), the onus is on the user to ensure proper use each time, which can lead to a higher failure rate with typical use compared to perfect use.
Allergic Reactions and Sensitivities
Latex Allergies: Latex condoms can cause allergic reactions in some individuals. Symptoms can range from mild irritation to more severe reactions, necessitating the use of alternative materials like polyurethane or lambskin, which have their own sets of pros and cons.
Spermicides and Irritation: Diaphragms are often used in conjunction with spermicidal gels, which can cause irritation or allergic reactions for some women, leading to discomfort or urinary tract infections.
Navigating the Downsides
Informed Choices: Users must be informed about these potential issues to make educated decisions about their contraceptive methods.
Alternative Options: For those who find the downsides of barrier methods outweigh their benefits, exploring other forms of contraception, such as hormonal methods or IUDs, may be advisable.
Barrier methods play an essential role in the contraceptive choices available to women. However, understanding their limitations is key to ensuring they are used effectively and comfortably, contributing to satisfying and worry-free sexual experiences.
Natural Family Planning and Fertility Awareness
Natural family planning (NFP) and fertility awareness-based methods involve tracking natural body signals to determine fertile and infertile phases of a woman’s menstrual cycle. While these methods empower women to understand and work with their bodies without the use of hormonal or physical contraceptives, they also come with significant challenges and require a high level of discipline and understanding.
Challenges of Accurate Fertility Tracking
Complexity of Cycle Tracking: Women must track their menstrual cycle daily, which can be complex and requires an understanding of bodily signals such as basal body temperature and cervical mucus. This complexity can lead to inaccuracies, especially in women with irregular cycles.
Time and Education: Properly utilizing NFP or fertility awareness methods requires significant time and education. Women need to learn about their cycles and understand how to interpret the signals, which can be a steep learning curve.
Discipline Required for Monitoring
Consistency in Tracking: These methods require daily monitoring and record-keeping, which can be burdensome and challenging to maintain consistently, especially during busy or stressful times.
Lifestyle Considerations: Lifestyle factors, such as irregular sleep patterns or illness, can affect body signals, making it harder to accurately track fertility.
Risk of Unintended Pregnancy
Higher Failure Rate with Typical Use: While fertility awareness methods can be effective with perfect use, the risk of unintended pregnancy is generally higher with typical use compared to other more reliable contraceptive methods. This is largely due to the challenges and potential for user error in tracking and interpreting fertility signals.
Navigating Natural Family Planning
Seeking Professional Guidance: It’s beneficial for women interested in NFP or fertility awareness methods to seek guidance from healthcare professionals or certified instructors to ensure they understand the techniques fully.
Combining with Other Methods: Some women choose to use barrier methods during the fertile phase to reduce the risk of unintended pregnancy.
Natural family planning and fertility awareness methods offer a hormone-free approach to contraception, aligning with the natural rhythms of the body. However, the effectiveness of these methods is highly dependent on accurate, consistent tracking and a deep understanding of one’s menstrual cycle, highlighting the need for thorough education and commitment.
Sterilization: Tubal Ligation
Tubal ligation, often referred to as having one’s “tubes tied,” is a form of permanent sterilization for women. It involves surgically closing or blocking the fallopian tubes to prevent eggs from reaching the uterus. While it is a highly effective form of contraception, it comes with considerations that are vital for women to understand before undergoing the procedure.
Permanence and the Risk of Regret
Permanent Solution: Tubal ligation is intended as a permanent form of contraception, making it a significant decision that requires careful consideration. Women must be sure that they do not want any more children in the future.
Potential for Regret: Some women may experience regret after the procedure, particularly if their life circumstances change. The risk of regret is higher among women who are younger, have fewer children, or undergo the procedure immediately following childbirth.
Post-Tubal Ligation Syndrome
Post-tubal ligation syndrome refers to a range of symptoms some women report after the procedure, including menstrual irregularities, hormonal changes, and increased menstrual pain. However, the existence of this syndrome is a subject of debate and research within the medical community. Women considering tubal ligation should discuss potential risks and side effects with their healthcare provider to make an informed decision.
Considerations for Tubal Ligation
Informed Decision-Making: It is crucial for women to receive comprehensive counseling about the implications of tubal ligation, including its permanence, the potential for regret, and the possibility of post-tubal ligation symptoms.
Alternatives and Reversal: Women should also consider alternative long-term but reversible contraceptive methods if there is any uncertainty about the decision. While tubal ligation can sometimes be reversed, the procedure is complex, and successful pregnancy after reversal is not guaranteed.
Tubal ligation offers a permanent solution for women who are certain they do not wish to have more children. However, the irreversibility of the procedure and the potential for regret or health complications necessitate thorough understanding and careful consideration before proceeding with this form of contraception.
Emergency Contraception
Emergency contraception is a crucial option for preventing pregnancy after unprotected sex or contraceptive failure. However, it’s essential to understand its proper use, potential side effects, and why it’s not a substitute for regular contraceptive methods.
Understanding Emergency Contraception
Purpose and Use: Emergency contraceptive pills (ECPs), often known as “morning-after pills,” are intended for use shortly after unprotected intercourse. They are not meant for regular contraceptive use but as a backup in unexpected situations.
Mechanism of Action: ECPs work by delaying ovulation, preventing fertilization, or stopping a fertilized egg from implanting in the uterus. The effectiveness of ECPs diminishes the longer the delay in taking them after unprotected sex.
Potential Side Effects
Immediate Side Effects: Women may experience side effects after taking ECPs, such as nausea, fatigue, headache, dizziness, breast tenderness, or irregular bleeding.
No Long-Term Risks: While the side effects can be uncomfortable, there are no known long-term health risks associated with the proper use of emergency contraception.
Misconceptions and Misuse
Not a Regular Method: A common misconception is that ECPs can be used as a regular form of contraception. This is not recommended due to the higher chance of failure compared to other contraceptive methods and the potential for side effects.
Educational Gap: There’s a need for better education and clear communication about the intended use of emergency contraception, ensuring that it’s understood as a last resort, not a primary method of birth control.
While emergency contraception is a vital tool in preventing unwanted pregnancy, it’s important for women to be fully informed about its proper use, potential side effects, and limitations. Healthcare providers play a key role in dispelling myths and providing clear guidance on the responsible use of emergency contraception.
Access and Societal Barriers
Access to contraceptives and accurate information about them is crucial for women to make empowered decisions about their reproductive health. However, various access issues and societal barriers can hinder the effective use and understanding of contraceptive methods, impacting women’s health and autonomy.
Access Issues
Availability and affordability: In some areas, certain contraceptive methods may not be readily available, or they may be cost-prohibitive. This lack of access can limit women’s choices and force them to rely on less preferred or less effective methods.
Healthcare Infrastructure: The quality of healthcare infrastructure, including the availability of trained healthcare providers and confidential services, can significantly affect access to contraceptives. Inadequate services can lead to misinformation and discourage women from seeking the care they need.
Societal Barriers
Cultural and religious beliefs: In many societies, cultural and religious beliefs can shape attitudes toward contraception, sometimes stigmatizing its use and leading to a lack of support for women who wish to use contraceptives.
Misinformation and Education: Misinformation about contraceptives can proliferate, especially in areas where comprehensive sex education is lacking. Myths and misconceptions about the safety and effects of contraceptives can deter their use and lead to unintended pregnancies.
Gender Dynamics and Autonomy: Societal norms about gender roles and autonomy can impact women’s ability to make decisions about their reproductive health. In some contexts, women may need to negotiate contraceptive use with their partners or face barriers in accessing contraceptives independently.
Addressing the Challenges
Improving Access: Efforts to improve access to contraceptives must address both the logistical aspects, such as availability and affordability, and the quality of healthcare services.
Educational Initiatives: Comprehensive sex education and public health campaigns can counteract misinformation, ensuring that women and the broader community have accurate information about contraceptive options and their use.
Empowering Women: Societal change is needed to empower women to make informed decisions about their reproductive health. This includes advocating for women’s autonomy, challenging stigmas associated with contraceptive use, and supporting women’s rights to access the healthcare they need.
Overcoming access issues and societal barriers is essential to ensuring that all women have the information and resources they need to make informed choices about contraception. Addressing these challenges requires a multifaceted approach involving healthcare improvements, educational initiatives, and societal change.
Conclusion
The journey through the various female contraceptive methods and their downsides illuminates the complex landscape that women navigate in making informed decisions about their reproductive health. Understanding the potential downsides of each contraceptive option is not intended to deter use but to empower women with comprehensive knowledge, ensuring that their choices align with their health needs, lifestyle preferences, and personal values.
Contraceptives play a pivotal role in enabling women to take control of their fertility and plan their futures. However, the decision-making process is nuanced and individual. It involves weighing the benefits against the potential downsides, from side effects and health risks to lifestyle impacts and access barriers. This process underscores the importance of open dialogue, thorough understanding, and careful consideration.
Healthcare providers play an indispensable role in this journey. They are not just sources of information but also advocates and allies. Their support is crucial in helping women navigate the complexities of contraceptive choices, addressing concerns, debunking myths, and tailoring recommendations to individual health profiles and life situations.