Does Contraceptive Play a Role in Infertility
In an era of family planning, the contraceptives has become part of life for many couples. If contraception is so efficacious and prevalent, it only shows we have come to need it. In addition to having been increasingly used, however, there are long-term doubts about whether this will, however inadvertently, affect fertility or bring on the derivative maladies. As millions contemplate choices about their reproduction and health, it is important to understand how they might materially affect them. This article delves into the heart of this concern, exploring various forms of contraceptives, from hormonal pills to intrauterine devices (IUDs), and barrier methods like condoms, and examining their relationship with long-term fertility. By dispelling myths and highlighting facts, we aim to provide clarity on how these methods influence, or do not influence, the ability to conceive in the future.
Different Types of Contraceptives
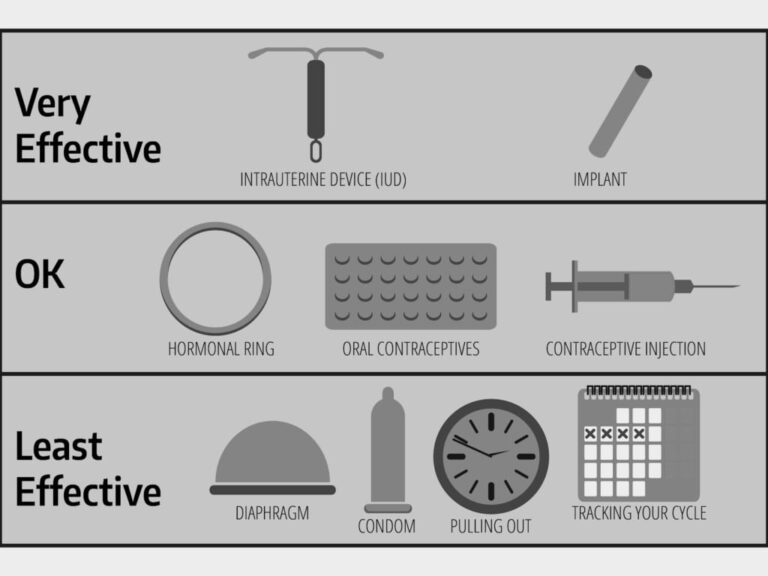
Contraceptive methods are diverse, each functioning uniquely to prevent pregnancy. Broadly, they can be categorized into hormonal, barrier, and natural methods, among others.
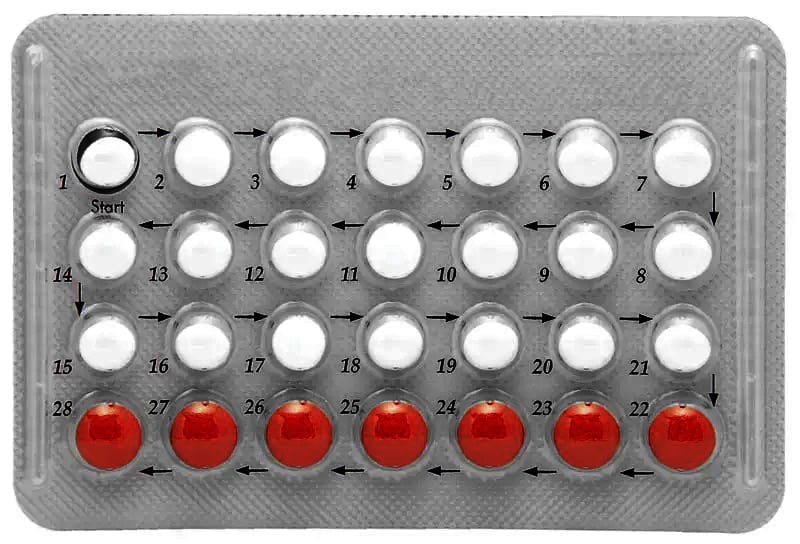
Hormonal Contraceptives: These include birth control pills, patches, injections, vaginal rings, and implants. They primarily work by releasing hormones like estrogen and progestin to inhibit ovulation, thicken cervical mucus to block sperm, and alter the uterine lining to prevent implantation. These methods are highly effective when used correctly and consistently.
Barrier Methods: These are the methods for blocking of the sperm to not reach to ova, using diaphragms, cervical caps, and contraceptive sponges and condoms, intra-uterine devices as a type of shield. Let us say, that male condoms are now widely recognized as the most common barrier method and indeed shield products being used in the world for sexual activity are invaluable protection against sexually transmitted diseases.
Natural Methods: This category encompasses methods like fertility awareness (tracking menstrual cycles to avoid sex during fertile days), withdrawal (pulling out), and lactational amenorrhea (breastfeeding as a form of contraception post-childbirth). While these methods involve no synthetic hormones or physical devices, their effectiveness heavily depends on proper and consistent practice.
Each contraceptive method has its own advantages and disadvantages and which choice to make often depends on personal health, lifestyle and family planning objectives. Understanding how each method works is key to making an informed choice when it comes to family planning and sexual health.
Hormonal Contraceptives and Fertility
Hormonal contraceptives, a popular method of birth control, work by altering the body’s natural hormones so that pregnancy cannot happen. Birth control pills, most often used, mostly contain both estrogen and progestin. Those pills stopping ovulation completely, they also make the mucous on a woman’s cervix different, making it difficult for sperm to get through to egg (a natural obstacle in itself).
Long-term effects on fertility of these methods are a topic of extensive research. Although it is true that hormones prevent pregnancy whilst used, research shows them to be quite quickly reversed once discontinued. According to the American College of Obstetricians and Gynecologists, most women return to their pre-pregnancy levels of fertility within a few months after stopping contraception, no matter how long they have been using it. Studies suggest also that pregnancy rates among those who have stopped hormonal contraceptives and those who have never started them are roughly the same one year later.
Non-hormonal contraceptives and fertility
Non-hormonal methods are actually quite different in their mechanism of preventing pregnancy. The most widely known non-hormonal methods include intra-uterine devices (IUDs), condoms and the diaphragm.
IUDs: Intrauterine devices, especially copper IUDs, are inserted into the uterus and prevent pregnancy by creating an environment that is toxic to sperm and eggs. Copper IUDs do not release hormones and are known for their long-term effectiveness. Studies have shown fertility returns quickly after use of IUDs are discontinued, with pregnant rates comparable to women who did not use IUDs at all.
Condoms: Male condoms, usually made of latex or polyurethane, physically block sperm from entering the womb. This only contraceptive method can also be used to prevent sexually transmitted diseases. Female condoms, which are inserted in the vagina, work by the same principle. There is no evidence that long-term use of condoms has any effect on fertility.
Diaphragms: These shallow, dome-shaped cups are inserted into the vagina to cover the cervix, preventing sperm from getting inside. Like condoms, diaphragms have no hormone components and thus do not affect a woman’s natural menstrual cycle or fertility.
Retracting Contraceptive Effects and the Time It Takes to Conceive
One very important consideration about using contraceptives is how soon after stopping you can expect to be able to conceive a child. It is important to note that individual experiences can vary, and factors like age, overall health, and specific reproductive health issues play a significant role in determining how quickly one can conceive after stopping contraception. While contraceptives do not typically have long-term effects on fertility, consulting with a healthcare provider for personalized advice is always recommended for those planning to conceive.
Get a help
If concerns arise about fertility after discontinuing contraceptives, it is important to know when to seek medical advice. Generally, it is advisable to consult a healthcare provider if pregnancy does not occur within one year of trying for women under 35 and within six months for women over 35. Additionally, if there are known pre-existing fertility issues, irregular menstrual cycles, or other health concerns that might affect fertility, seeking earlier medical consultation is recommended. A healthcare provider can offer guidance, conduct necessary assessments, and discuss potential fertility treatments if needed.
Conclusion
From contraception to conception, there are many choices and considerations along the way. This discussion reveals that while contraceptives do effectively prevent pregnancy, their impact on long-term fertility is generally reversible. Most people will regain their fertility shortly after stopping contraceptive use. However, it is important to bear in mind that individual experiences can vary Case by case. Issues like age and overall health are significant factors in fertility. As they press on down the path, and know they can rely on contraceptives tried and true means to plan families.