Diabetes and pregnancy
Diabetes during Pregnancy
Diabetes in pregnancy, including gestational diabetes and pre-existing diabetes (Type 1 and Type 2), present substantial risks and challenges. Gestational diabetes, manifesting during pregnancy, and pre-existing diabetes can have negative implications for both maternal and fetal well-being. Effective management of blood sugar is essential for minimizing the potential complications, which include premature labor, preeclampsia, and the hazards associated with high birth weight. This article outlines the types of diabetes that can develop during pregnancy and how they diagnosed. Their potential impact on maternal and fetal health, including risks to the pregnancy, and their effective management, including protocols for postpartum care.
Understanding Diabetes in Pregnancy
Diabetes during pregnancy can be as gestational or pre-existing diabetes. Gestational diabetes is diabetes that develops during pregnancy and disappears after the baby is delivered. It usually occurs when the body cannot produce enough insulin to meet the extra needs of pregnancy. Pre-existing diabetes is diabetes that a woman already has before she becomes pregnant. It includes type 1 and type 2 diabetes. The major difference between these types is the timing of their onset. Gestational diabetes is specifically related to pregnancy and to the hormonal changes and hyperinsulinemias of pregnancy, whereas pre-existing diabetes is a pre-existing condition that the patient had before her pregnancy. Pregnancy can make pre-existing diabetes more difficult to control due to hormonal changes that affect blood sugar levels. On the other hand, well-controlled diabetes—whether gestational or pre-existing—can assure the healthiest pregnancy and baby for the mother.
Risk Factors and Diagnosis of Gestational Diabetes
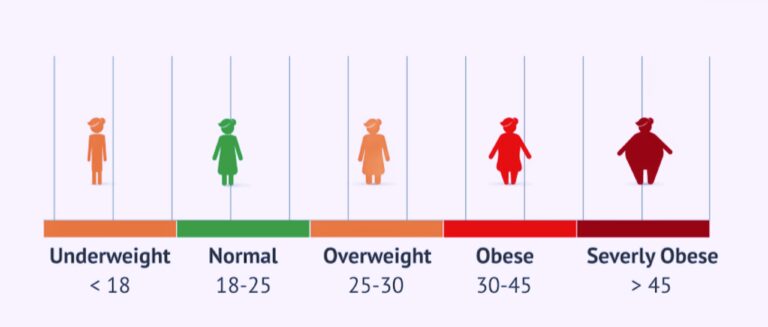
Gestational diabetes can develop in any pregnant woman, but certain factors increase the risk. These include:
1. Being over the age of 25.
2. Having a family history of diabetes.
3. being overweight.
4. Having had gestational diabetes in a previous pregnancy.
Women from Asian, Hispanic, African, and Native American backgrounds are also at higher risk.
Screening for gestational diabetes is a routine part of prenatal care. It typically involves a glucose challenge test, where blood sugar levels are measured after drinking a sweet liquid. If the test shows high blood sugar, a follow-up glucose tolerance test is done for a definitive diagnosis.
The screening is usually performed between the 24th and 28th weeks of pregnancy. However, women with high risk factors may be screened earlier in their pregnancy to ensure any issues are identified and managed promptly.
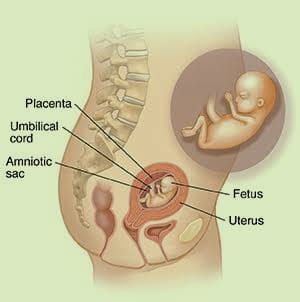
Impact on Pregnancy and Fetal Development
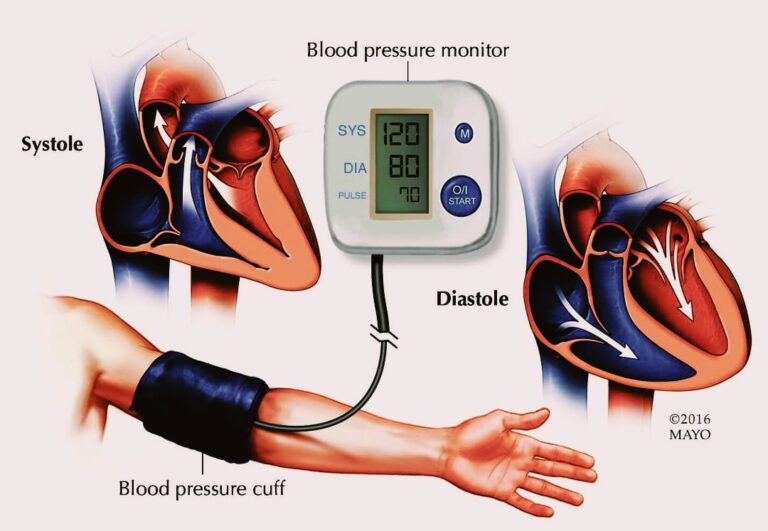
Both short- and long-term consequences are associated with having diabetes while pregnant. In the short term, it can result in conditions such as high blood pressure or preeclampsia, which can be severe if not managed appropriately. In the long term, women who have gestational diabetes are at a higher risk of developing Type 2 diabetes down the road.
For the fetus, uncontrolled blood sugar levels can lead to concerns. These include higher risks of premature birth, excess birth weight, and respiratory distress syndrome.
The baby could also develop low blood sugar (hypoglycemia) after being born. Additionally, children born to mothers with poorly controlled diabetes during pregnancy have a greater risk of developing obesity and Type 2 diabetes themselves. As a result, it is important to keep blood sugar levels well controlled during pregnancy for both the health of the mother and the baby.
Management Strategies for Diabetes in Pregnancy
Dietary Management
A variety of foods in a balanced diet is the best way to manage diabetes during pregnancy. This means eating whole grains, fruits, vegetables, lean proteins, and healthy fats. Because a pregnant woman’s body is working to maintain a stable environment for the fetus, she may feel the symptoms of hypoglycemia or low blood sugar more acutely. Smaller, more frequent meals can help keep blood sugar stable and symptoms at bay. For tips and guidance on meal planning and understanding carbohydrate, protein, and fat balance, consult a dietitian or nutritionist.
Physical Activity
Regular exercise is a crucial component of effective diabetes management. Aerobic exercise can help control blood sugar levels. Walking, swimming, and prenatal yoga are all generally safe and effective types of exercise for pregnant women with diabetes. It’s always best to talk to a healthcare provider before beginning any new exercise regimen, but this is especially important during pregnancy. An obstetrician can help determine what kind of exercise is appropriate, taking into account a woman’s individual health status and the characteristics of her pregnancy.
Blood Glucose Monitoring
Consistently high blood sugar levels are especially dangerous for the developing fetus. Pregnant women with diabetes should test their blood sugar levels as much as their healthcare provider recommends. For some women – particularly those with gestational diabetes – the frequency of testing might increase during pregnancy. Healthcare providers may set different targets for blood glucose levels during pregnancy than under other conditions, so women should aim to meet the specific guidelines set by their healthcare providers. A healthcare provider or diabetes educator can help a pregnant woman learn to test and adjust her insulin, diet, and exercise based on the results of the test.
Medication and Insulin Therapy during Pregnancy
For some women, medication and insulin therapy are an important part of managing diabetes during pregnancy. When diet and exercise aren’t enough to keep blood sugar levels within targets, medication or insulin is often necessary. Because insulin doesn’t cross the placenta, it is the first choice for treating gestational diabetes, making it the most commonly used medication for diabetes during pregnancy. Glyburide or metformin are additional oral medications for gestational diabetes that are occasionally used. Healthcare providers monitor evidence about the safety of these medications very carefully, so the guidance on their use can change.
It is common for the type and dose of insulin to change during pregnancy. In addition to being affected by lifestyle changes like diet, exercise, and work schedule like anyone else, a pregnant woman’s blood sugar levels may also be affected by hormonal changes. The dose of insulin she needs can change frequently, and she may need to work with her healthcare provider regularly to adjust her dose. With increased testing and careful consideration, women with diabetes can maintain safe blood sugar levels during pregnancy. There is no absolute safe level of blood sugar at any time during pregnancy, but keeping levels as close to normal as possible protects both the mother and the baby.
It is important for pregnant women to work closely with their healthcare team to determine the best medication strategy for their specific needs.
Monitoring Maternal and Fetal Health
Regular prenatal check-ups are vital for monitoring the health of both mother and baby during a diabetes-affected pregnancy. These appointments allow healthcare providers to track fetal growth and well-being, ensuring the baby is developing normally.
Women with diabetes during pregnancy may need additional tests or ultrasounds to closely monitor fetal development and detect any potential issues early. These can include specialized scans to assess the baby’s size and heart function. Keeping up with these appointments helps in managing diabetes effectively and ensuring a healthy pregnancy outcome.
Preparing for Delivery with Diabetes
Managing diabetes during pregnancy also involves planning for delivery. The timing of delivery is carefully considered, as women with diabetes are often encouraged to deliver by their due date or sometimes earlier, depending on their health and the baby’s condition.
During labor and delivery, blood sugar levels are closely monitored to ensure they remain stable. This is crucial for both the mother’s and the baby’s health.
After delivery, it is important to continue monitoring blood sugar levels, as they can fluctuate significantly in the postpartum period. This helps in adjusting any diabetes management plans and ensuring a safe recovery for the mother.
Postpartum Care and Future Considerations
After delivery, breastfeeding is encouraged as it can help regulate blood sugar levels. However, women with diabetes should monitor their blood sugar closely, as insulin requirements may change during breastfeeding.
Women who have had gestational diabetes are at an increased risk of developing Type 2 diabetes later in life. Regular health check-ups and maintaining a healthy lifestyle are important to reduce this risk.
Educate Yourself
Learning about the condition and how to manage it can go a long way in helping women with gestational diabetes manage their health. Many hospitals and clinics offer gestational diabetes education, and having access to a dietitian for meal planning and a diabetes educator for learning the disease process and self-management is essential.
Commit to a Balanced Diet
Sticking to a healthy, well-balanced diet is essential when managing diabetes, especially during pregnancy. Eating whole foods and avoiding processed foods and sugar-filled drinks can significantly improve blood sugar levels.
Follow Through with Postpartum Care
After delivering her baby, a woman who had gestational diabetes should stay connected to her healthcare provider and schedule the appropriate postpartum care and follow up. Remaining engaged with healthcare providers after pregnancy can help ensure good health for mother and baby in the long-term.
Preparing for future pregnancies
Keep in mind that one of the most crucial strategies when it comes to future pregnancies is early planning and health optimization. Preconception counseling can help with the effective management of diabetes so that next time, the outcome of pregnancy may be even healthier.
Support and Resources for Diabetes Management in Pregnancy
Emotional support and counseling are crucial for women facing diabetes in pregnancy. It can be overwhelming and sometimes accessing mental health resources and counseling can make a world of difference.
Educational resources and support groups can also be invaluable in terms of information and peer support. Groups can be found through many hospitals and clinics, as well as online, allowing women to share their experiences and advice with one another.
Finally, a dedicated healthcare team that may include doctors, nurses, dietitians, and diabetes educators is an essential part of the equation. Their knowledge and guidance through pregnancy and into the postpartum period is invaluable when it comes to managing diabetes effectively and ensuring the health of both mother and baby.
Conclusion
Effectively managing diabetes in pregnancy is essential for the health and well-being of both mother and child. Proactive, follow-through care and listening to medical advice can significantly reduce the risks of diabetes in pregnancy. It is critical that women follow up with their healthcare providers, not only during pregnancy, but also postpartum to ensure ongoing health for themselves and their babies. Remember, taking steps to lead a healthy lifestyle and reaching out for support as needed are essential to success in pregnancy and long-term health for mother and baby.