Joints And Back Pain in Pregnancy
Joint pain during pregnancy can be caused by a variety of reasons, such as weight gain, hormonal fluctuations, and the body’s adaptation to support the growing baby. In the elbows, fingers, knees, hips, and other flexing areas of your body, you may experience stiffness, discomfort, or pain.
Causes
Many things can cause joint pain during pregnancy. The most common causes of joint pain in expectant mothers are:
- Weight gain is an effect of growing a small human. Increased weight puts more stress on bones and joints, increasing the likelihood of joint pain.
- Hormonal changes Uncertainty and discomfort can result from ligament and joint flexibility, especially when the level of relaxation is increased.
- Posture changes Pregnancy also increases the likelihood of joint pain due to changes in body weight. A mother’s posture may change as her belly grows to accommodate her growing baby, which can result in hip and lower back pain.
Symptoms
- Pregnant women often experience joint pain, stiffness and pain in the fingers, ankles, knees, elbows and hips.
- Increased pain when standing, sitting, or moving around for long periods of time.
- Swelling and inflammation around injured joints.
- Inability to perform normal tasks such as walking around and climbing stairs.
Exercise Tips Pain Relieve Joints Pain during Pregnancy
- Low-impact exercises like walking, stationary cycling, and yoga for pregnant women, and swimming.
- Exercises to strengthen the muscles that support your joints, especially the lower back, hips and pelvis, should be the main focus of your strength training program.
- Use of ice packs, heating pads, or baths provide hot and cold treatments.
- Wear supportive shoes
- Take daily breaks to rest the body.
- Prenatal Fitness Classes through safe and effective exercises designed specifically for pregnant women.
Back-pain in Pregnancy
Back pain is one of the most common problems related to pregnancy. More than 50% of women suffer from some degree of back pain. Physical changes related to pregnancy, such as altered hormone levels, changes in the center of gravity, and altered posture, are responsible for most back pain.
According to studies, lower back pain often starts between 5 and 7 months of pregnancy, while sometimes it can start as early as the 8 or 12 weeks.
Causes
There are several variables that contribute to this discomfort:
- Changes in hormones: Your body produces a hormone called relaxin during pregnancy, which causes the joints to loosen and the pelvic ligaments to relax in preparation for childbirth. This same hormone can cause the ligaments that support the spine to loosen, resulting in pain and instability.
- Weight Gain: A growing baby causes a shift in your center of gravity, which puts pressure on your back muscles.
- Posture Change: Poor posture, prolonged standing and bending over can trigger or worsen back pain.
- Stress: Stress increases in weak parts of the body. Your back pain may worsen during the stressful times of your pregnancy due to changes in your pelvic floor.
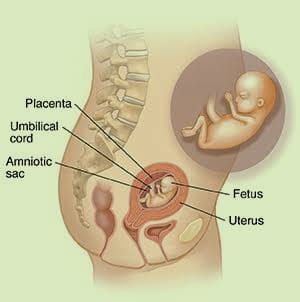
- Separation of muscles: A muscle known as the rectus abdominis, which extends in two parallel sheets from the rib cage to the pubic bone, can tear along the medial suture as the uterus grows. Distance can make back pain worse.
Diagnosis
To determine your range of motion and level of pain, your healthcare professional may examine your legs, hips, and back. Your pregnancy and previous back problems may be their questions. To rule out alternative causes of back pain, imaging procedures such as MRI and X-ray may be recommended in certain circumstances.
Treatments
Pay attention to your posture when you sit. Nothing strains your spine more than spending all day in a chair. Make sure the chairs you use frequently, both at home and at work, provide adequate support. Preferably, they should have a straight back, arms, and firm cushions. Don’t cross your legs; Instead, elevate your feet slightly using footrests. This can cause your pelvis to tilt forward, which puts more strain on your back muscles.
- Exercise: Regular exercise increases strength and flexibility. As a result, your spine may experience less stress. Static cycling, walking, and swimming are safe exercise options for most expectant mothers. Your physical therapist or doctor may recommend exercises to strengthen your back and abdomen.
- Proper Posture: Try to adopt good posture while working, sitting or sleeping as bad posture can lead to back strain. You can relieve pressure on your back by sleeping on your side and placing a pillow between your knees. Keep your feet up, sit up straight, and keep your shoulders back using a pillow behind your back for support. Using a brace or support belt may also be beneficial.
- Heat and Cold therapy: Your back may benefit from warm-ups and cool-downs. If your doctor allows it, start applying cold compresses (a bag of ice or frozen vegetables wrapped in a towel) to the sore area several times a day for 20 minutes at a time. Change in temperature after two or three days; Use a heating pad or hot water bottle on the injured area. Be careful not to overheat your belly when you are pregnant.
- Wear Supportive Shoes: To keep your posture straight and reduce stress on your back, choose supportive, comfortable shoes.
- Stretch Regularly: Look for “come back stretch,” “back stretch,” and “standing pelvic tilt.” These strengthen your back and lower back muscles.
- Counseling: If stress aggravates or worsens your back pain, counseling may be helpful. A counselor or therapist will listen to your thoughts and feelings and help you process your emotions and manage stress. Consult your physician for more details or counseling recommendations.
- Chiropractic or Acupuncture: A chiropractor or acupuncturist may be able to help some women with back pain. Nevertheless, it is important to speak with a health care professional before trying any alternative treatment.