Infertility Due to Ova Deformity after Age 35 in Women
As women embark on the journey of life, one of the most significant biological transformations they face pertains to fertility. Especially notable are the changes that occur in female fertility as a natural consequence of aging, particularly after the age of 35. This critical age threshold marks not just a symbolic milestone but also a pivotal point in reproductive health. The quality and quantity of ova, the egg cells vital for conception, undergo significant changes as women cross into their late thirties. These alterations have profound implications for conception, pregnancy, and overall reproductive health. Understanding how ova are affected by age is not just a matter of scientific interest but a crucial aspect of informed family planning and reproductive decision-making. As such, gaining insight into the age-related changes in ova can empower women with the knowledge needed to navigate their fertility journey with greater awareness and preparedness.
Understanding Ova and Aging
Ova, or egg cells, are the cornerstone of female reproductive capability. Each ovum represents the potential beginning of a new human life when fertilized by sperm. These cells are unique in their biological role; they carry half of the genetic material required for the development of an embryo and, eventually, a child. Unlike men, who produce new sperm continuously, women are born with a finite number of ova. This ovarian reserve is established even before birth, and no new egg cells are produced during a woman’s life.
As women age, their ova also undergo a natural aging process, which is distinctly different from the aging of other cells in the body. While most body cells can repair themselves or are replaced regularly, ova do not have this capability. They age as a woman ages, gradually decreasing in both quantity and quality over time. The decline in quantity is a straightforward reduction in the number of available eggs. In terms of quality, the aging ova are more likely to develop chromosomal abnormalities, which can lead to difficulties in conception and potential complications in pregnancy. This aging process of ova is inexorable and significantly influences a woman’s fertility landscape, especially as she reaches her mid-thirties and beyond.
Changes in Ova after Age 35
The transition beyond the age of 35 marks a significant shift in a woman’s reproductive biology, particularly concerning the ova. The most prominent change is in the ovarian reserve, the pool of available eggs a woman has. As a woman ages, the number of eggs in her ovarian reserve naturally diminishes. This decrease is not only in quantity but also in the quality of the ova that remain. By the time a woman reaches her mid-thirties, the decline becomes more pronounced, leading to a reduced likelihood of successful conception.
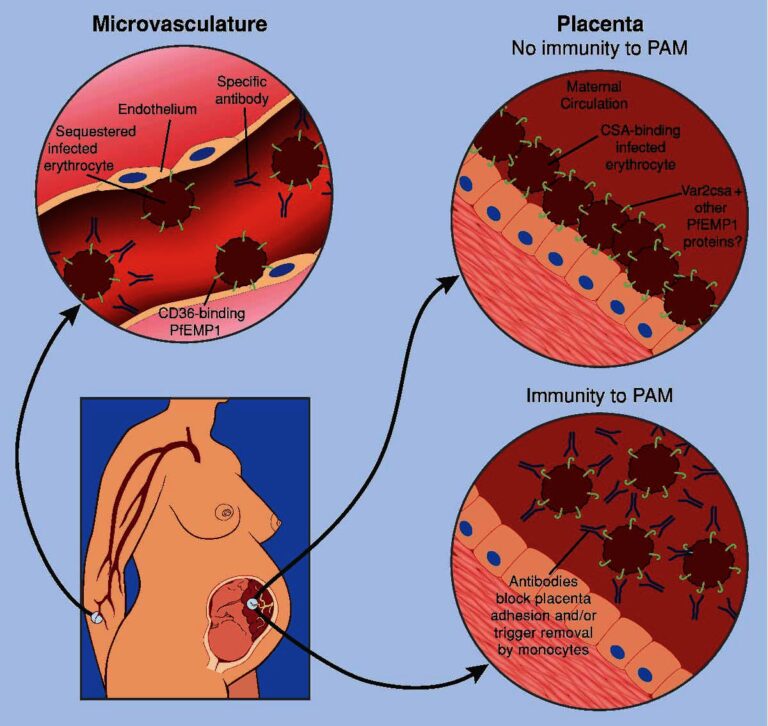
Quality deterioration in ova primarily involves genetic integrity. As women age, the likelihood of chromosomal abnormalities in their eggs increases. This can result in conditions like Down syndrome, where an extra chromosome is present in the baby’s genetic makeup. These chromosomal abnormalities are largely due to errors in a process called meiosis—the type of cell division that results in eggs and sperm. In older ova, errors during meiosis become more common. These errors can lead to eggs with an abnormal number of chromosomes (aneuploidy), significantly impacting fertility and the potential health of the embryo.
The implications of these changes are far-reaching. Reduced egg quantity means fewer opportunities for successful fertilization, while diminished quality raises the risks of infertility, miscarriage, and chromosomal disorders in offspring. This natural age-related decline in both the quantity and quality of ova is a critical factor for women to consider as they plan their families in their thirties and beyond.
Impact on Fertility and Pregnancy
The age-related changes in ova significantly impact a woman’s fertility and the potential outcomes of pregnancy. One of the most immediate effects of these changes is an increased difficulty in conceiving. As women age, particularly after 35, the reduced quantity and compromised quality of ova lower the chances of successful fertilization. This decline in fertility is a gradual process but becomes more pronounced with each passing year, often leading to a higher risk of infertility.
The quality of ova not only affects the ability to conceive but also the health of the pregnancy. Older ova are more prone to chromosomal abnormalities, which can lead to a range of complications. One of the most common implications is an increased risk of miscarriage. The body often naturally terminates pregnancies that have significant genetic issues, and the likelihood of such issues is higher with older ova.
Additionally, pregnancies conceived with older ova have a higher risk of resulting in genetic disorders such as Down syndrome. Down syndrome, or trisomy 21, is a condition where the baby has an extra copy of chromosome 21. The probability of having a baby with Down syndrome increases with maternal age, particularly after the age of 35. This rise is directly linked to the higher incidence of chromosomal anomalies in older ova.
It is important for women and couples to be aware of these risks when planning a pregnancy later in life. While many women successfully conceive and deliver healthy babies after 35, understanding the potential challenges can help in making informed reproductive choices and preparing for possible medical interventions or genetic counseling.
Options and Strategies for Older Women
For women over 35, several options can aid in conception. Assisted reproductive technologies (ART) like in vitro fertilization (IVF) can significantly increase the chances of pregnancy. IVF, often used in combination with preimplantation genetic testing, can help select embryos with the best chance of a healthy pregnancy. Egg donation is another viable option, especially for those facing severe egg quality issues. Additionally, early fertility assessments and counseling can provide valuable insights into individual fertility status and guide decision-making. These proactive steps can empower older women in their pursuit of motherhood.
Conclusion
Navigating the challenges of fertility with advancing age, particularly the impact of ova quality and quantity, requires both understanding and resilience. While the journey may present unique obstacles, the array of modern fertility solutions offers hope and possibility. For women facing these challenges, remember that each journey is personal and choices abound. Empowerment through knowledge, combined with medical advancements, paves the way for many to achieve their dreams of parenthood.