Infertility & Insurance by State & Major Insurance Companies + Federal Law
Introduction
Infertility, defined as the inability to conceive after a year of regular, unprotected intercourse, touches millions of lives, with profound emotional and financial ramifications. The journey to parenthood, for many, is tarnished by the challenge of infertility, turning what should be a time of hope into a period of stress and uncertainty. The medical interventions designed to combat infertility, though often effective, come with high costs that can be prohibitive without adequate insurance coverage.
This reality casts a spotlight on the crucial role that insurance coverage plays in the realm of infertility treatments. Coverage for procedures like in vitro fertilization (IVF) can alleviate financial burdens, making the dream of parenthood more accessible. However, navigating the labyrinth of insurance policies adds another layer of complexity.
With the landscape of insurance coverage for infertility treatments varying widely between states and among insurance providers, understanding the interplay of state laws, policies of major insurance companies, and federal regulations is paramount. This article seeks to dissect these multifaceted issues, providing a comprehensive guide to the current state of insurance for infertility treatment in the United States. We will delve into the specific mandates that govern state-level coverage, scrutinize the policies of major insurance carriers, and demystify the impact of federal regulations, all with the aim of equipping those facing infertility with the knowledge to navigate their options effectively.
As we embark on this exploration, the significance of advocacy and informed decision-making becomes clear, understanding the intricacies of insurance coverage is not just a practical necessity but also a vital aspect of the fight against infertility.
Understanding Infertility
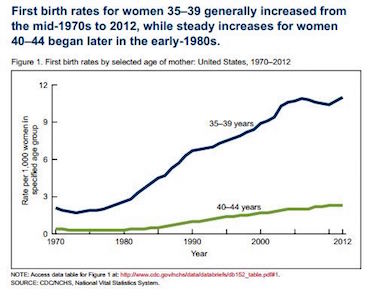
Infertility, a condition that impedes the ability to conceive, is clinically defined as the failure to achieve a successful pregnancy after 12 months or more of regular unprotected intercourse. The World Health Organization recognizes infertility as a disease, a definition that underscores its severity and the importance of access to treatment. This period for diagnosis is shortened to six months for women over the age of 35, due to the natural decline in fertility associated with aging.
The Medical Criteria and Causes
Infertility can be primary (where a couple has never conceived) or secondary (where the couple has conceived in the past but is currently unable to do so).
Common causes in women include ovulatory disorders, fallopian tube damage, endometriosis, and uterine or cervical anomalies. In men, infertility may be due to low sperm production, abnormal sperm function, or blockages that prevent sperm delivery.
Lifestyle factors like smoking, excessive alcohol use, obesity, and stress can also affect fertility, as can environmental toxins and certain medical treatments such as chemotherapy.
Available Treatments
Treatments range from medication to stimulate ovulation to more advanced techniques like assisted reproductive technology (ART). ART includes procedures like IVF, intrauterine insemination (IUI), and third-party assisted techniques like sperm donation and surrogacy.
Surgical interventions may be required to rectify anatomical issues, and fertility preservation strategies such as egg or sperm freezing are increasingly used, particularly among those undergoing treatments that may compromise their future fertility.
Prevalence of Infertility
Statistics indicate that infertility affects approximately 10% to 15% of couples of reproductive age globally. In the United States, about 1 in 8 couples have trouble getting pregnant or sustaining a pregnancy.
Infertility is not gender-specific; it affects men and women equally. Approximately one-third of infertility is attributed to female factors, one-third to male factors, and the remaining third to a combination of problems in both partners and unexplained causes.
Understanding infertility’s definitions, causes, and treatments is fundamental for those navigating this challenge. While the journey may be fraught with complexities, medical science offers a ray of hope, with ongoing advancements providing new avenues for achieving successful pregnancies.
Insurance Coverage for Infertility by State
Navigating the landscape of infertility insurance in the United States reveals a patchwork of regulations, with coverage mandates varying significantly from state to state. As of now, only a select number of states have laws requiring insurance coverage for infertility treatment, which includes diagnostic procedures, treatments like IVF, and sometimes medication.
States with Mandated Coverage
States like Illinois, Maryland, Massachusetts, and New Jersey are among those with the most comprehensive mandates, requiring certain insurers to cover a wide range of infertility treatments.
These mandates often stipulate the inclusion of several cycles of IVF, which can be a crucial factor in the success of infertility treatment, given that multiple cycles are often necessary.
Types of Coverage Provided
Coverage can include initial fertility assessments, ovulation induction treatments, IUI, IVF, egg and sperm retrieval procedures, and associated lab work.
Some states extend coverage to include egg or embryo freezing when medically necessary, such as before cancer treatment that could affect fertility.
Coverage for fertility preservation for non-medical reasons, like elective egg freezing for age-related fertility decline, is less commonly mandated.
Limitations and Exclusions
State mandates typically apply only to insurers that fall under the jurisdiction of state insurance regulators, meaning self-insured employers, which are federally regulated, may opt out.
Many states have specific requirements that must be met for coverage to apply, such as defined periods of infertility or a certain number of attempted natural or IUI cycles before IVF is covered.
Additionally, some states exclude certain populations from coverage, like single individuals or same-sex couples, though recent legislative efforts have aimed to remove such exclusions.
Discrepancies in Coverage
The level of mandated coverage can vary widely. For instance, some states might cover only diagnosis and treatment but not the actual ART procedures, while others may have caps on the amount they will pay or the number of treatment cycles covered. Certain states require specific diagnostic criteria to be met or that individuals have specific insurance plans.
The complexity of state mandates for infertility insurance coverage reflects a broader conversation about access to healthcare and reproductive rights. With the cost of infertility treatments often being prohibitively expensive, state-mandated coverage can be a lifeline for many. However, the limitations and exclusions present in these mandates mean that the financial burden of infertility remains a significant obstacle for many Americans.
Major Insurance Companies and Their Policies on Infertility Coverage
When it comes to infertility coverage, the policies of major insurance companies are as varied as the conditions they insure. Understanding the nuances of these policies is crucial for individuals navigating the challenging terrain of infertility treatments.
Coverage Options Offered
Most major insurance companies offer a range of plans, some of which include infertility treatment coverage. These options typically cover diagnostic procedures to determine the cause of infertility and may cover treatments like hormone therapy or surgery.
Coverage for ART, including IVF, is more variable. Some insurers’ offer it as part of the standard package, while others provide it as an add-on or not at all. Plans may differ in the number of treatment cycles covered and whether additional procedures like ICSI or embryo cryopreservation are included.
Comparative Analysis
Company A may offer comprehensive infertility coverage but with high premiums and deductibles, making it less accessible despite its broad benefits.
Company B might provide more coverage that is limited but with lower out-of-pocket costs, presenting a more affordable though restricted option.
The differences extend to network restrictions, with some companies maintaining a preferred provider network that limits where patients can receive covered services.
Case Studies and Coverage Scenarios
A case study might illustrate a couple with coverage through Company C that only covers three cycles of IVF, after which they had to switch to a more expensive plan or pay out of pocket for additional cycles.
Another scenario may involve an individual whose plan through Company D covers diagnostic procedures but not the cost of treatment, leaving them to finance costly ART procedures independently.
Navigating Policy Specifics
It is not common for the same insurance company to offer different levels of coverage in different states, depending on state mandates and market demands.
Fertility coverage can also be affected by the size of the employer through which the insurance is provided. Large corporations may have more advantage to negotiate comprehensive coverage for their employees.
Importance of Understanding Individual Policies
For those seeking infertility treatment, a thorough understanding of their specific policy is essential. It is not just about whether infertility treatment is covered, but to what extent and under what conditions.
This understanding can significantly affect financial planning and treatment decisions. Knowing the policy details can also prepare individuals for potential appeals or negotiations with insurance providers.
The policies of major insurance companies regarding infertility coverage are a critical piece of the puzzle for individuals striving to build their families. With each policy presenting a unique set of provisions, limitations, and opportunities, the importance of careful review and understanding cannot be overstated.
Federal Laws and Infertility Coverage
While state mandates significantly shape the fertility insurance coverage landscape, federal laws also play a pivotal role. The Affordable Care Act (ACA), enacted in 2010, brought sweeping changes to health insurance in the United States but stopped short of mandating infertility coverage nationwide.
The Affordable Care Act’s Influence
The ACA established essential health benefits that must be covered by new insurance plans, yet it did not specifically list infertility treatments as one of these benefits.
However, the ACA did influence infertility coverage indirectly. For instance, it prohibited discrimination based on pre-existing conditions, including infertility, and required plans to cover many of the basic services involved in diagnosing and treating infertility.
Interaction with State Mandates
Federal law does not preempt state mandates on infertility coverage. This means that in states with existing mandates, insurance plans must comply with both federal ACA requirements and state-level infertility coverage laws.
For employer-sponsored plans, especially those that are self-insured, coverage is often governed by the Employee Retirement Income Security Act (ERISA), a federal law that supersedes state mandates. However, these plans may still opt to provide infertility benefits.
Recent Legislative Changes
Recent legislative efforts, like the proposed Access to Infertility Treatment and Care Act, aim to expand infertility coverage under federal law. If passed, it would require more health plans, including those offered by the federal government, to provide infertility treatment coverage.
Additionally, the Family Act has been introduced in Congress multiple times and seeks to create a tax credit for the out-of-pocket costs associated with infertility medical treatment.
Implications of Federal Legislation
The implications of federal legislation on infertility coverage are significant. Should new laws be enacted, they could standardize coverage across states, providing more equitable access to infertility treatments.
This would not only ease the financial burden on individuals seeking such treatments but could also influence the cost of treatments across the healthcare industry.
The interplay between federal laws and state mandates creates a complex regulatory environment for infertility coverage. While the ACA provided a framework for essential health benefits, the lack of federal mandates specifically for infertility treatments leaves a gap that state laws and private insurance policies must fill. Understanding these laws and their implications is crucial for anyone navigating the infertility treatment process.
The Financial Burden of Infertility Treatments
The cost of infertility treatments can be staggering, often constituting a significant financial burden for couples without insurance coverage. Treatments like in vitro fertilization (IVF), while offering hope for many struggling with infertility, come with a hefty price tag that can reach into the tens of thousands of dollars.
The Cost of IVF in Detail
In the United States, the average cost of a single IVF cycle runs between $12,000 and $17,000. The exact price will depend on where you live, what clinic you use, and what specific requirements your treatment has.
The cost of medicine (typically $1,500 to $3,000 a cycle), special tests and procedures like intra-cytoplasmic sperm injection (ICSI) or pre-implantation genetic diagnosis (PGD) are all additional charges.
For numerous couples, several IVF cycles are needed. The business and financial hardships increase exponentially.
Other Infertility Treatments
Simpler treatments such as IUI cost less per cycle ($1,000 on average), but have lower success rates that might require more tries if you want an equivalent level of fertility and total costs rise accordingly.
Also adding to the total cost of fertility treatment are drugs taken for ovulation promotion or prior to IVF, since most of these are not covered by insurance.
Financial Fallout from No Insurance Coverage
If you have no insurance, the full cost of infertility treatment comes straight out-of-pocket, putting a serious dent into savings or potentially leading one into significant financial indebtedness.
The financial stress can also magnify the emotional and psychological impacts associated with infertility, influencing well-being as well as relationships.
Considerations for Financial Planning
For many couples, other financial channels come into play, such as obtaining loans in order to afford treatments, payment plans offered by doctors or clinics, grants provided by non-profit groups and sometimes even a combination of these forms of funding.
Some states have assistance programs of their own, while certain clinics use income-sensitive fee scales or shared risk packages; these latter may provide a partial refund if treatment fails.
Inequity in access to reproductive health can be seen through the high cost of infertility treatment. On the other hand, such costs also underscore how truly crucial it is for comprehensive health insurance policies to include coverage of infertility treatments if earning of individuals are going have any chance at creating their own families. As talk of health care reform goes on, it remains a major topic for the people.
Advocacy and Future Directions in Infertility Insurance Coverage
Advocacy groups are at the forefront to expand infertility treatment coverage. Their tireless efforts to get the high financial costs of infertility onto government attention agendas have made sure that cost is not their only focus. However, the groups are also working hard for fair access to reproductive care.
The Work of Advocacy Groups
Organizations such as RESOLVE: The National Infertility Association and the American Society for Reproductive Medicine (ASRM) are on the front lines for those suffering infertility.
These groups lobby both state and federal governments to mandate insurance coverage, provide aids to understanding policies for affected individuals, and offer advice on working with policymakers.
Potential Future Changes in Coverage
As part of comprehensive health reform, more and more states are moving toward mandating coverage for infertility. Advocates are calling for existing mandates to be more comprehensive and for further mandates in other states. On the federal level, proposed bills currently before Congress might require that all insurance providers cover infertility procedures. If so, this could make treatment available to everyone in every walk of life.
Influencing Policy through Public Opinion and Political Action
Public opinion can push lawmakers into implementing new policy. In tandem with this trend, societal knowledge about infertility problems and sympathy for sufferers has been increasing.
People who campaign also make use of the power of personal storytelling, so advocacy organizations encourage just such a practice.
Political action also incorporates voting, and voters are beginning to recognize that candidates carrying reproductive health messages, including infertility coverage, will have their support.
The Vital Role of Continued advocacy
The future of fertility coverage hinges on sustained advocacy efforts. Successful expansion of coverage often follows years of persistent lobbying, education, and negotiation.
Community support and visibility are of the essence. Events like National Infertility Awareness Week help to correct misconceptions, reduce stigma, and gather public pressure for national insurance that covers infertility treatments.
How to Navigate Infertility Treatment Insurance
Understanding the complexities of insurance for infertility treatment can appear daunting. However, knowing how your specific coverage works and when to advocate for yourself make a big difference. Here are some practical suggestions for couples:
Understanding Your Insurance Plan
Know your coverage: Thoroughly review your insurance policy to determine what is covered and what is not. In particular, read carefully the sections of the policy dealing with infertility treatment, including diagnostic procedures, medications, and ART.
Ask Questions: If you have any questions or doubts, call up your insurance provider and ask. Be specific about things like how many cycles are covered and what prerequisites exist for coverage, as well as any exceptions that might apply to this or that treatment.
Keep Detailed Records: Keep a detailed record of all communication with your insurance company, including whom you spoke to, dates and times of calls, as well as any advice given by the insurance provider.
Advocating for coverage
Be persistent: If your plan includes any form of infertility coverage, such as paying all costs, persist to ensure that you receive what your rightful benefits entitle you to. Do not be disheartened by initial denials; those can often be turned over on appeal later.
Know the Appeals Process: Be familiar with your insurer’s appeals process. This could involve a formal letter of appeal, additional medical information, or a review by a third-party arbitrator.
Appeal of Insurance Denials
Gather the Documents You Will Need: When preparing to appeal a denial, gather the necessary documents. This includes your medical records, letters from your healthcare provider explaining the necessity of treatment, and those sections of your policy that are relevant to your situation.
Write a Compelling Letter of Appeal: Compose a clear and convincing letter to present your case. Cite policy language and specific medical evidence. Stress the need for treatment with compelling medical reasons along with long-term savings potential for infertility treatment costs. Support the needs of those seeking solutions to their insurance problems.
Get Support: Reach out for support. Your healthcare provider’s office may have experience dealing with insurance companies and be able to provide you valuable advice. Advocacy groups are another source of support and help.
Understanding insurance, taking effective action, and appealing denials allows for a greater chance of receiving the extended assistance needed when seeking infertility treatment.
Conclusion
The struggle to achieve pregnancy treatment is an arduous route full of emotional, physical, and financial hardship. The significance of comprehensive insurance coverage in this journey cannot be overstated: It is not only a financial cushion but also a light of hope that enables many people to pursue these dreams of parenthood. Without it, costs for treatments such as IVF would make them too expensive for most people overall.
Now the infertility insurance terrain in the US is a complicated mosaic marked by inconsistencies and inequities. Many major insurance companies’ policies vary, as do state mandates. These complex realities suggest that there is an essential need for information, direction, and fierce struggle: have it on good authority that every breakthrough in coverage has come from understanding the system, staying stubbornly on even ground, and speaking collectively for what we know is right. Tomorrow’s improvements will be achieved in that same way.