Bacterial Meningitis in Newborns
Bacterial meningitis is a serious and potentially life-threatening infection of the protective membranes covering the brain and spinal cord (meninges). In newborns, this condition requires urgent medical attention due to the risk of severe complications and high mortality rates. This article provides an overview of bacterial meningitis in newborns, including its causes, symptoms, diagnosis, treatment, and preventive measures.
What is Bacterial Meningitis
Bacterial meningitis is an infection caused by bacteria that leads to inflammation of the meninges. In newborns, the condition can progress rapidly and cause severe outcomes, including neurological damage and death.
Causes of Bacterial Meningitis in Newborns
Common Pathogens
Group B Streptococcus (GBS): One of the most common causes of early-onset bacterial meningitis in newborns, typically acquired during delivery from the mother.
Escherichia coli (E. coli): A significant cause of early-onset meningitis, especially in preterm infants.
Listeria monocytogenes: Can cause meningitis, particularly in newborns whose mothers have eaten contaminated food.
Haemophilus influenzae type b (Hib): Although less common due to widespread vaccination, it can still cause bacterial meningitis.
Neisseria meningitidis: Known for causing meningococcal meningitis, though less common in newborns compared to older children and adults.
Streptococcus pneumoniae: Can also cause meningitis in newborns, though more frequently in older children.
Transmission Routes
Perinatal Transmission: Newborns can acquire bacterial pathogens from the mother during childbirth if the mother is colonized or infected.
Postnatal Transmission: Infections can also be acquired from other infected individuals or contaminated surfaces.
Symptoms of Bacterial Meningitis in Newborns
Classic Symptoms
Symptoms of bacterial meningitis in newborns can be subtle and may include:
Fever or Hypothermia: Elevated body temperature or abnormally low temperature.
Poor Feeding: Difficulty in feeding or refusal to feed.
Lethargy: Excessive drowsiness or irritability.
Vomiting: Frequent or persistent vomiting.
Bulging Fontanelle: The soft spot on the top of the baby’s head may appear swollen or bulging.
Seizures: Seizures or convulsions may occur.
Hypotonia: Reduced muscle tone, leading to floppy or weak limbs.
Additional Signs
High-Pitched Cry: A distinctive, high-pitched cry that can indicate distress.
Respiratory Distress: Difficulty breathing or irregular breathing patterns.
Jaundice: Yellowing of the skin and eyes, particularly in severe cases.
Diagnosis of Bacterial Meningitis
Clinical Evaluation
Diagnosis begins with a thorough clinical evaluation:
Medical History: Assessment of maternal health, delivery history, and any potential exposure to infectious agents.
Physical Examination: Detailed examination to identify symptoms consistent with meningitis.
Diagnostic Tests
Several tests are essential for confirming the diagnosis:
Lumbar Puncture (Spinal Tap): The primary test for diagnosing meningitis, where cerebrospinal fluid (CSF) is collected from the spinal canal and analyzed for signs of infection, including elevated white blood cells, protein levels, and decreased glucose levels.
Blood Cultures: To identify the causative bacteria and assess for other infections.
Imaging Studies: CT scans or MRIs may be used to evaluate the extent of infection and rule out other conditions.
Polymerase Chain Reaction (PCR): For detecting specific bacterial DNA or RNA in CSF or blood.
Treatment of Bacterial Meningitis
Antibiotic Therapy
Immediate antibiotic treatment is crucial
Empirical Antibiotics: Broad-spectrum antibiotics are administered as soon as bacterial meningitis is suspected, before the specific pathogen is identified. Common choices include cefotaxime or ceftriaxone combined with vancomycin or ampicillin.
Targeted Therapy: Once the specific bacteria are identified, treatment may be adjusted based on susceptibility testing to more targeted antibiotics.
Supportive Care
Oxygen Therapy: To maintain adequate oxygen levels and support respiratory function.
Intravenous Fluids: To ensure proper hydration and electrolyte balance.
Anticonvulsants: Medications to manage seizures if they occur.
Pain Management: Addressing discomfort and providing supportive care to the infant.
Monitoring and Follow-Up
Continuous Monitoring: Regular assessment of vital signs, neurological status, and response to treatment.
Follow-Up Care: Monitoring for potential complications and ensuring complete recovery, including developmental assessments.
Preventive Measures
Maternal Screening and Treatment
Group B Streptococcus Screening: Testing and treating pregnant women for GBS to reduce the risk of transmission to the newborn.
Prenatal Care: Regular prenatal visits to identify and manage potential infections.
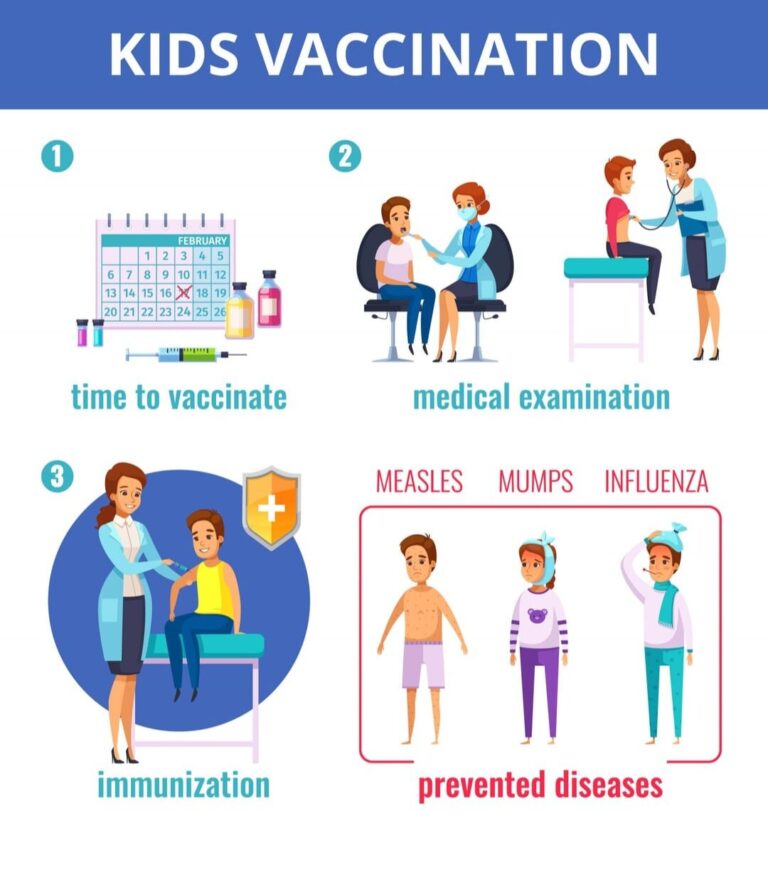
Vaccination
Routine Vaccinations: Ensuring that infants receive recommended vaccinations, including the Haemophilus influenzae type b (Hib) and pneumococcal vaccines, to protect against common bacterial pathogens.
Hygiene and Infection Control
Hand Hygiene: Practicing rigorous handwashing protocols in healthcare settings and by caregivers.
Isolation Precautions: Implementing appropriate isolation measures for infected individuals to prevent the spread of infection.
Long-Term Outlook
The prognosis for bacterial meningitis in newborns depends on several factors:
Early Treatment: Prompt and effective treatment improves outcomes and reduces the risk of severe complications.
Complications: Potential long-term effects include neurological impairment, developmental delays, or hearing loss, especially if the infection is severe or treatment is delayed.
Recovery: Many infants recover fully with appropriate medical care, but regular follow-up and developmental assessments may be necessary.
Conclusion
Bacterial meningitis in newborns is a critical condition that demands immediate medical attention. Early diagnosis through clinical evaluation and diagnostic tests, combined with prompt antibiotic therapy and supportive care, is essential for managing the infection and minimizing complications. Preventive measures, such as maternal screening, vaccinations, and stringent hygiene practices, play a vital role in reducing the risk of bacterial meningitis and ensuring the health and well-being of newborns.