Pregnancy — BMI
Introduction
Body mass index (BMI) is not just a simple number, but a significant measure of public health. Importantly, it also happens to be a critical index in pregnancy: for women who are about to begin this journey in their life understand thoroughly how BMI works? And what its implications? It affects not only their ability to conceive children but all of prenatal life as well and has a bearing on their own health beyond childbirth. It is the duty of each of us to take into account women’s BMI.
Measuring body fat in terms of height and weight provides a standardized index which is helpful for judging unhealthy points of people who are underweight, overweight from a health perspective of BMI. In the case of pregnant women, a woman’s BMI has an impact on her ability to get pregnant, the possibility of gestational diabetes and developmental abnormality in the fetus. For this reason, it is also one of the important items in prenatal checkups and treatments.
To realize the significance of BMI during pregnancy is more than just achieving arbitrary numbers; it is for health that one begins living a healthy lifestyle with attention to balance. A woman’s BMI before or at some stage in pregnancy is fundamental to her whole person profile of health. This means equilibrated attention and active habits supporting Mother and child both need to achieve top-rate results.
Understanding BMI
BMI, or body mass index measures a person’s weight in kilograms divided by the square of their height in meters. It is a widely used way of categorizing individuals that can tell us something about their health risk level based on where they fall within certain weight ranges.
Calculations and Criteria
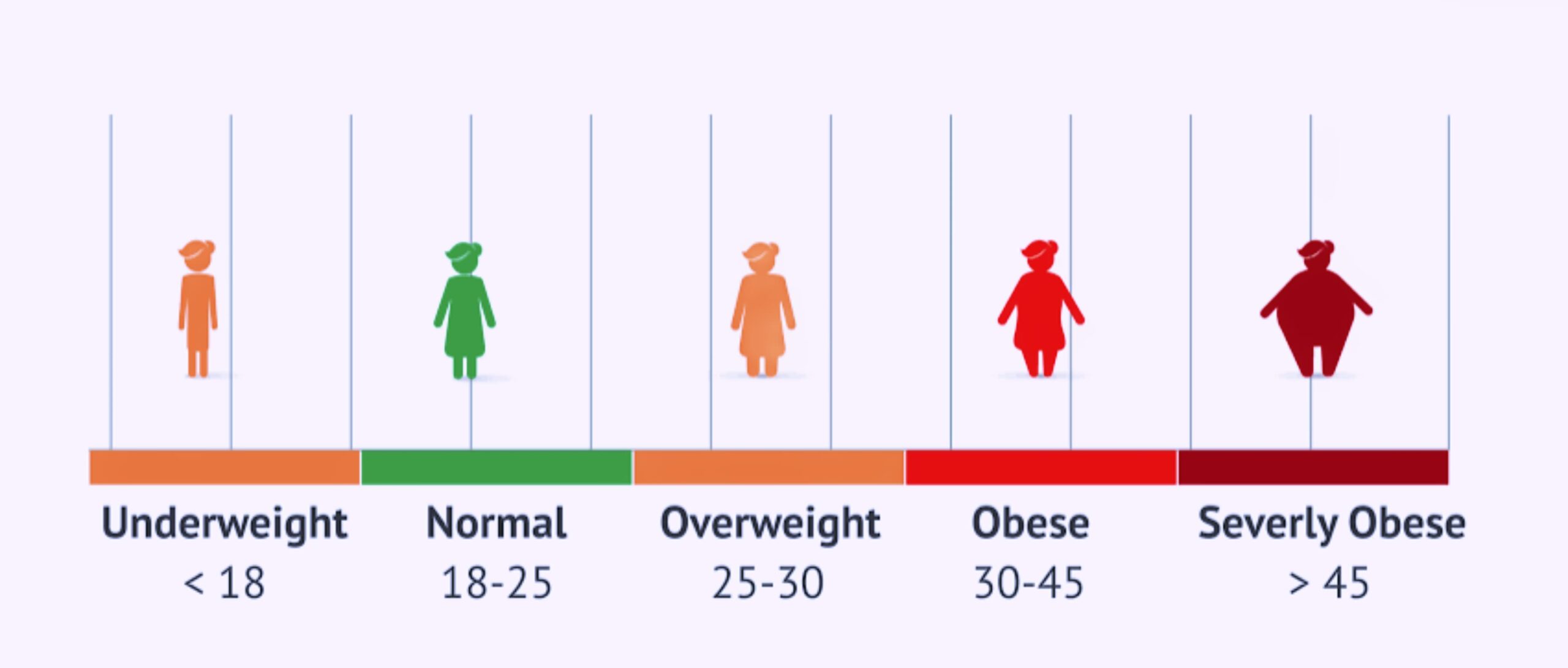
Formula: BMI is calculated as weight in pounds divided by the square of the height in inches. You can also use metric units: [weight (kg) / [height (m)]^2].
Categories: The resulting number places individuals in several categories: underweight (BMI less than 18.5), normal weight (BMI 18.5-24.9), overweight (BMI 25-29.9), and obese (BMI 30 or greater).
Healthy BMI for Childbearing Women
Mean BMI ranges: The mean BMI for females of childbearing age ranges between 18.5–24.9. However, the range also depends on variables such as age, muscle mass, and ethnic background.
Reasons: Maintaining a BMI inside this range is typically accompanied by easier fertility outcomes and less dangerous pregnancy and childbirth experiences.
BMI plays a part as an opening screening tool, making a rapid estimate of a woman’s condition in relation to her weight. The importance of BMI in pregnancy planning is critical because it has a direct impact on the health of women, her experience of pregnancy, and the health of her future offspring.
BMI Recommendations for Pregnancy
It is particularly important when planning for pregnancy to sustain a healthy Body Mass Index (BMI). The suggested BMI ranges for women who are preparing to conceive are instrumental in not only the ability to become pregnant but also the health of the pregnancy and the baby.
Optimal BMI Ranges for Conception and Pregnancy
Recommended Ranges: Typically it is suggested that women should maintain a BMI which is somewhere between 18.5 to 24.9 when trying to become pregnant. This is associated with the best outcomes for fertility and pregnancy.
Why Healthy Weight Is Essential: This optimum weight enables women to regulate menstrual cycles and ovulation which are necessary for conceiving. It also cuts down on the risk of pregnancy complications and birth problems.
Risks of Deviating from Recommended BMI
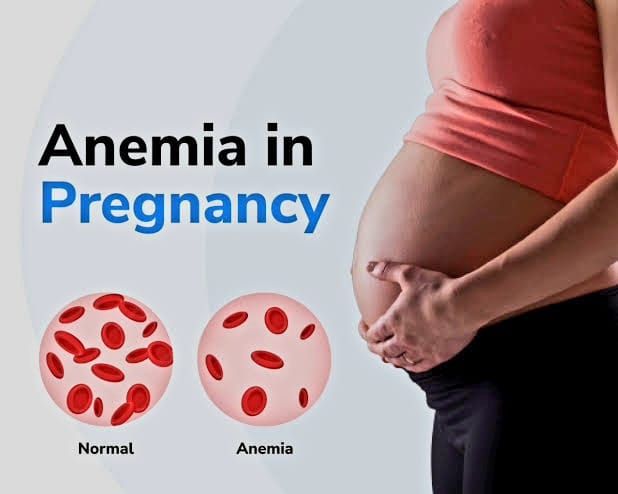
Underweight Threats: With a BMI lower than 18.5, menstrual cycles and ovulation become irregular making it more difficult to get pregnant. It also increases the risks of preterm delivery and having a baby with low birth weight.
Overweight and obese risks: A BMI above 24.9 can be associated with increased rates of infertility, as well as higher chances of pregnancy complications like gestational diabetes, preeclampsia, and cesarean delivery. For the child, it raises the risk of future obesity and health issues.
Studies show that the emphasis placed upon pre-pregnancy and pregnancy BMI is supported by a great deal of data. Before doing an orderly fertility procedure, women need to keep their weight under control through both balanced nutrition and regular exercise. Throughout pregnancy itself these same healthy lifestyle habits should continue, not just for the mother’s own health but also that of her baby.
IBMI Charts and Interpretation
BMI charts can be used as a helpful reference to monitor weight status. They show where an individual falls within the range of weight categories and therefore act like guidelines for those planning their pregnancy.
Using BMI Charts
Designed for Women: In BMI charts for women, gender considerations are usually included. When using these charts, it is essential that the correct one designed for women is chosen, as differences in body composition between genders can affect BMI.
Interpretation: The BMI category is generally displayed on one axis of the chart and height on another, with weight used as their inter-measurement variable. By locating the point on two sides where different weights meet, one can learn what their exact BMI category is.
Practicality in Pregnancy Planning
Preconception Health: Women in the preconception stage are helped by BMI charts to decide what weight category is healthiest for both fertility and pregnancy health.
Healthcare providers may use modified BMI charts during pregnancy to determine whether pregnant women are within a healthy range for gaining weight. Its proper management not only helps baby grow better but also minimizes problems with the mother’s health.
To visualize BMI-weight relationship as an aide during consultations in clinical settings, medical practitioners employ BMI charts to help clear up the meaning of BMI for her childbearing patients. With modern advances in technology, digital BMI calculators and telephone apps offer users tailor-made tracking and advice, making it possible for women to monitor their BMI from home. BMI charts are more than a set of numbers on a grid. By providing a clear image of how a woman’s weight stacks up against her height, these charts serve as encompass to help guide her as well as that of her future children.
Influence of BMI on Fertility and Pregnancy Progression
Fertility Considerations: A BMI that is either too low or too high can disrupt hormonal balance, which can impede ovulation and diminish fertility. Women with a BMI outside the recommended range may find they take longer to become pregnant. BMI plays a vital role in a woman’s fertility, her pregnancy course and the health outcomes for both mother and fetus. In order to anticipate and manage potential risks and complications, it is important to gain understanding of the impact of BMI on one’s future prospects.
Pregnancy Progression: When a woman becomes pregnant, her BMI still has significant impact on how it proceeds. Proper weight gain according to pre-pregnancy BMI needs to be achieved, in order to support the baby’s growth and let mother stays health. Women may be born with either low or high BMI but cannot gain height, and do themselves wrong from the start by starting off too low or not high enough.
BMI and Fetal Development
Mother’s body condition is much related to the supply of nutrients to the fetus. Underweight women may be unable to offer sufficient energy resources for optimal growth, meaning undernutrition in fetuses; and correspondingly overweight women will bring about excess levels of blood sugar with larger birth weights for their unborn babies.
Potential Future Problems: Emerging studies point to a possible link between the mother’s BMI and long-term health risks for her children. Children are more likely to develop metabolic disorders as adults if their mother has a higher body mass index (BMI) during pregnancy.
Complications Linked to BMI Categories
Underweight Risks: Women with low BMI face increased risks of preterm birth, delivering babies with low birth weight, and potential developmental delays.
Overweight and Obesity Risks: High BMI is associated with gestational diabetes, preeclampsia, higher chances of cesarean delivery, and postpartum hemorrhage. Babies born to mothers with high BMI are at increased risk for premature birth, high birth weight, and childhood obesity.
Managing BMI: For women with BMI outside the recommended range, healthcare providers typically offer guidance and support to reach a healthier weight before conception or manage weight gain during pregnancy appropriately.
The importance of maintaining a healthy BMI for a safe pregnancy and positive health outcomes for both mother and child cannot be overstated. It is a critical component of pre-pregnancy care and prenatal health that requires attention and action from both expecting mothers and their healthcare providers.
Managing BMI for Pregnancy
Achieving and maintaining a healthy BMI is a crucial step for women preparing for pregnancy or already pregnant. Proper management of BMI through diet, exercise, and lifestyle choices can significantly impact maternal and fetal health. Both preconception and prenatal periods offer opportunities for women to optimize their health, supported by the guidance of healthcare professionals.
Guidance on Managing BMI
Balanced Diet: A balanced, nutrient-rich diet is foundational. It should include a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. Portion control and understanding nutritional content help in maintaining a healthy weight.
Regular Exercise: Moderate exercise, as recommended by a healthcare provider, can help maintain a healthy weight and reduce the risk of pregnancy complications. Activities can include walking, swimming, prenatal yoga, or other low-impact exercises.
Lifestyle Choices: Avoiding harmful substances such as tobacco and excessive alcohol, managing stress, and ensuring adequate sleep are all essential lifestyle factors that contribute to a healthy BMI.
Support from Healthcare Professionals
Preconception Counseling: Healthcare professionals can offer valuable advice during preconception visits, helping women understand how their current BMI impacts their fertility and pregnancy and setting realistic goals for achieving a healthy weight.
Monitoring During Pregnancy: Regular prenatal visits allow for monitoring of weight gain, ensuring it stays within healthy parameters for the pregnancy stage. Healthcare providers can offer personalized advice based on the individual’s BMI, dietary habits, and activity level.
Postpartum Support: Guidance doesn’t stop after delivery. Support for returning to a healthy weight postpartum is also crucial, ensuring long-term health for the mother and setting a strong foundation for future pregnancies.
Managing BMI for pregnancy is a dynamic process, requiring a personalized approach and ongoing support. Healthcare professionals play a vital role in guiding, educating, and supporting women through this journey, helping to ensure the best possible outcomes for both mother and baby.
Societal Perspectives and Support Systems
Societal attitudes towards weight, particularly in the context of pregnancy, can significantly influence women’s perceptions and behaviors. Misconceptions and pressures surrounding weight can pose challenges, yet a supportive healthcare system and society are instrumental in fostering healthy BMI practices among women of childbearing age.
Addressing Societal Pressures and Misconceptions
Pressure to Fit a Mold: Women often face societal pressures to maintain a certain body image, which can be intensified during pregnancy. It’s important to challenge these norms and emphasize that a healthy pregnancy can look different for each individual.
Misconceptions about Weight and Fertility: Common misconceptions can lead to undue stress or unhealthy practices. Clear, factual information about the actual impact of BMI on fertility and pregnancy health is crucial to dispel myths and encourage a more informed and self-compassionate approach.
Importance of a Supportive Healthcare System
Accessible Information and Resources: A healthcare system that provides accessible, clear information and resources about managing BMI can empower women to make informed decisions about their health.
Individualized Care: Healthcare providers should offer individualized care and support, recognizing that each woman’s journey with BMI, pregnancy, and health is unique.
– Postpartum Support : Beyond pregnancy, support should extend into the postpartum period, helping new mothers navigate the physical and emotional changes, including returning to a healthy BMI.
Fostering a Supportive Society
Community Support: Building communities, both online and offline, where women can share experiences, advice, and encouragement can be incredibly beneficial. These communities can offer a counter-narrative to harmful societal pressures and foster a culture of support and understanding.
Education and Advocacy: Ongoing education and advocacy are needed to address and shift societal perceptions about weight, pregnancy, and health. This involves not just providing information but also actively working to change the conversation around these topics.
Conclusion
The journey of pregnancy is profoundly influenced by a multitude of factors, among which BMI stands out as a crucial determinant of maternal and fetal health. This exploration of BMI in the context of pregnancy underscores the importance of understanding, managing, and supporting healthy BMI practices, not only as a personal health goal but also as a societal imperative.
Maintaining a healthy BMI is pivotal for ensuring optimal fertility, a smooth pregnancy, and the well-being of both mother and baby. It’s about striking a balance – nourishing the body for its incredible task of creating new life while also safeguarding one’s health. The relationship between BMI and pregnancy is complex, intertwined with factors ranging from fertility and pregnancy progression to the long-term health of the child.