Male Vasectomy: Why, How Much of Success, vs How Much of Cost.
Introduction
On the landscape of family planning and contraceptive options, vasectomy represents a significant, if often incomplete or misunderstood, alternative. It is, after all, a permanent choice and more deliberate than turning toward other methods. However, it is no surprise that the method’s popularity is on the upswing, nearly decades after its first day of use; market trends attribute its broader use to its growing effectiveness, minimal invasiveness, and one-time cost.
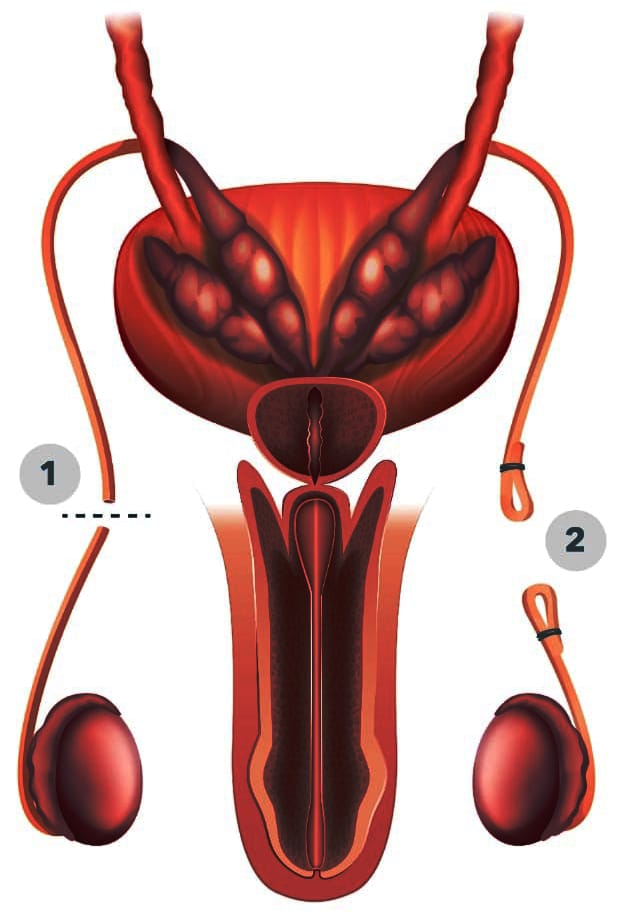
Vasectomy is a surgical procedure for male sterilization in which the vas deferens are cut and sealed off, the tubes that carry sperm from the testicles to the urethra, where they are combined with other fluids to create semen. It’s a pretty straightforward procedure, usually done in a doctor’s office or an outpatient setting under local anesthesia, that’s known for a quick recovery and prodigious benefit.
The decision to take a vasectomy as a form of contraception is deeply personal and generally made due to a variety of contributing factors, among them: the couple has determined that their family size is complete; desire for a method of contraception that is permanent rather than reversible; consideration for the health and well-being of a partner. Invasive female procedures are in turn allowing men to take a greater responsibility in birth control.
The concept of a minimally invasive irreversible procedure is appealing to many, as is the freedom for their partners to avoid contraceptive procedures altogether. This collective decision, by both couples or individuals, involves significant elements of one’s control and comfort with managing fertility; studies show that it’s for this reason that men opt for the procedure more so than any other including female sterilization in order to take control of their reproductive destiny. As many men would say, it’s simply less of an invasive procedure for them. The permanence of vasectomy, however, is a two-sided coin; it offers the security of a long-term solution, but more so it also risks the future family planning desires.
Understanding the implications, effectiveness and (lack of) frequency of reversal are key factors to take when someone wants that.
What is vasectomy?
A vasectomy is more than a mere medical procedure. It is a choice that is often made by men and women in concert as a significant moment in a man’s reproductive life.
How it is Performed?
Vasectomy involve cutting or blocking the vas deferens, the tubes that carry sperm from the testicles to the urethra, so the sperm no longer mixes with semen and is ejaculated. The procedure is generally swift, consisting of roughly 20 to 30 minutes.
Types of Vasectomy
There are essentially two types of vasectomy — the traditional technique, which involves making very small incisions, and the no-scalpel vasectomy, which is done without incisions by using a tiny puncture to get to the vas deferens. Both methods are highly successful, and the choice can depend on the surgeon’s experience and the preference of the patient.
Purpose and Effectiveness
Contraception
The clear aim of a vasectomy is to provide permanent contraception. It is one of the most successful forms of birth control, with a success rate of over 99 percent.
Non-impact on Sexual Function
It is important to note that a vasectomy will not affect a man’s sexual intercourse, his ability to have an erection, the feeling of having an orgasm, or the volume of the ejaculate; the only difference is that the ejaculate will no longer contain sperm.
Permanence and Reversibility
A Permanent Decision
While a vasectomy is intended to be a permanent form of contraception, it is important for individuals to be comfortable with proceeding. Couples are often advised to consider all factors, including the possibility of different life circumstances and a change of heart concerning future children.
Potential for Reversal: Vasectomy reversal is possible but is a more complex surgery than a vasectomy and the success of a reversal depends on several factors including how long it has been since the vasectomy. Still, it is important to approach a vasectomy with the mindset that it is a permanent solution.
Understanding a vasectomy from the procedure itself to what it could mean long term in a man’s life is essential for anyone considering this form of contraception. It’s not a one-off medical procedure; it’s a significant life decision that requires careful thought and comprehensive consultation with healthcare professionals.
Why Men Choose Vasectomy
Choosing to have a vasectomy is an important decision and very much ‘a personal choice’ influenced by a combination of personal, psychological, and social factors. Men have any number of reasons why they opt not to retain the ability to have children and the decision-path to choosing this permanent form of contraception is as unique as they are.
Family Planning and Permanency
Completed Family Size: Once men have the number of children they decide they want, many will opt for a vasectomy to eliminate any possibility of more children. This decision is often made to establish and maintain a stable family situation and is often made because of financial considerations for the welfare of a growing family.
Permanency: Simplicity and the concept of a ‘final solution’ may appeal many. Men who are sure they do not want any further children might see the permanent nature of the vasectomy as ‘a line in the sand’ in relation to such matters. Having no desire for any further ‘contraception maintenance obligations,’ some men who are equally certain they do not want more child will see it as a solution that eradicates the issue for the last time.
Convenience and Effectiveness
Compared to other forms of contraception, a vasectomy is relatively simple and convenient. It is a one-time procedure with no ongoing maintenance, unlike birth control methods that require daily attention or periodic renewals. The reliability of vasectomy as a contraception method is a compelling factor. Its success rate is one of the highest among all contraception methods, offering peace of mind to those seeking a definitive solution.
Psychological and Social Considerations
A vasectomy can be seen as an empowering choice that allows a man to take control of his reproductive capacity and make a proactive decision about his future. Men may also choose vasectomy as an alternative out of consideration for their partners, particularly if the woman has experienced side effects from other forms of contraception or if a health condition makes other forms of contraception contraindicated. For some people, vasectomy is the responsible choice not only for their family, but also in a broader social context. They may recognize the way that population growth contributes to strain on global resources and the environment, and having a smaller family may be a way for them to make a positive impact.
Influencing Factors
The decision to have this procedure can be heavily influenced by cultural background and societal norms. It is more common in societies where it is socially acceptable. In those where there is stigma or misinformation about vasectomy, the decision may be less common. Many personal factors influence family planning choices, including beliefs about family, desire for children, parenting philosophies, and the feeling of responsibility to family.
Making a vasectomy decision that you feel confident and positive about, is personal and important. It is critical to look into what is involved in the procedure so you can feel good about it. We are at a time in history when men are expected to play a wider role in family planning than before, so men are considering it under new expectations.
Cost and Financial Considerations
In addition to being a personal, medical and emotional choice, electing for a vasectomy is a financial burden as well. The cost of the process can vary based on location, the specific clinic or surgeon, as well as insurance.
Cost Breakdown of Vasectomy
The cost of the procedure can vary widely. It usually ranges between $300 and $3,000. The variance is based on method (conventional vasectomy or no-scalpel vasectomy), the experience of the surgeon, and the facility in which the procedure is performed. Initial consultations, assessments and pre-procedure tests may or may not be additional. These costs should be part of the overall budget for the vasectomy procedure. After the vasectomy is over, the vasectomy doctor requires follow-up appointments and sperm analysis tests. The sperm analysis tests are in place to ascertain that the vasectomy was a success and no sperm are present in the semen; this fact confirms the success of the vasectomy.
Insurance Coverage
Many insurance plans cover the cost of a vasectomy as it is considered a cost-effective method of contraception. However, the extent of coverage can vary. It is essential to check with your insurance provider about what is covered, including the procedure itself, consultation fees, and follow-up tests. For those without insurance or with plans that do not cover the procedure, understanding the out-of-pocket costs is important. Some clinics offer financing plans or sliding scale fees based on income to help manage these expenses.
Financial Assistance Programs
In some cases, state programs or non-profit organizations may offer financial assistance or reduced-cost services for vasectomy procedures. These can be particularly helpful for individuals without insurance or with limited financial resources. Navigating the financial aspects of getting a vasectomy requires careful consideration and planning. It is advisable to conduct thorough research, consult with multiple clinics, and communicate with your insurance provider to fully understand the costs involved. By doing so, individuals can approach this significant decision with clarity and confidence, ensuring that the financial implications are well within their planning and expectations.
Success Rates and Effectiveness
Vasectomy is renowned for its high success rate and reliability as a contraceptive method, making it a popular choice for many seeking permanent birth control. Understanding the effectiveness of the procedure, the likelihood of success, and the potential for complications is crucial for anyone considering this option.
High Success Rate
Vasectomy boasts a success rate of over 99%, making it one of the most effective forms of contraception available. The success of the procedure is measured by the absence of sperm in the semen after a certain period post-surgery. It is important to note that the effectiveness of a vasectomy isn’t immediate. Patients are usually required to undergo sperm analysis tests several months after the procedure to confirm that no sperm are present in the ejaculate. Until this confirmation, alternative contraception methods should be used.
Low Rate of Failure
While the failure rate of vasectomy is very low, typically less than 1%, it’s not nonexistent. Failures can occur due to improper surgical technique, recanalization (where the vas deferens manages to “heal” itself and become unblocked), or early post-vasectomy sexual activity before the sperm has been completely cleared from the semen. To minimize the risk of failure, it’s crucial for patients to attend all follow-up appointments and adhere to the guidelines provided by their healthcare provider, including semen analysis to confirm the absence of sperm.
Potential Complications
Most complications associated with vasectomy are minor and may include swelling, bruising, infection, or temporary discomfort at the site of the procedure.
More serious complications, such as chronic pain or sperm granuloma (a small, hard lump that forms due to sperm leakage), are relatively rare. The risk of these complications can be further minimized by choosing an experienced surgeon and following all post-operative care instructions.
Vasectomy’s high success rate and low rate of complications make it an appealing choice for many. However, the decision to undergo this procedure should always be made with a comprehensive understanding of its effectiveness, the need for follow-up, and the potential risks, ensuring that the choice aligns with one’s long-term family planning goals and personal circumstances.
Vasectomy Reversal
While a vasectomy is generally regarded as a permanent form of contraception, life circumstances and personal desires can change, leading some to consider vasectomy reversal. Understanding the process, its effectiveness, and the factors influencing its success is essential for those contemplating this decision.
Possibility and Process of Vasectomy Reversal
The most common form of vasectomy reversal is vasovasostomy, a surgical procedure that reconnects the severed vas deferens.
In more complex cases, a vasoepididymostomy may be required. This procedure connects the vas deferens directly to the epididymis, typically, when a blockage is present.
Both procedures require microsurgery, performed under a microscope to ensure precision. The surgery is more complicated and lengthier than the original vasectomy.
Effectiveness and Success Rates
The success of vasectomy reversal is measured by the return of sperm to the ejaculate and the ability to achieve pregnancy. Success rates can vary widely, generally ranging from 40% to 90%, depending on various factors.
The time elapsed since the original vasectomy is a significant factor. Reversals performed within ten years of vasectomy generally have higher success rates. Other factors include the age of the patient and their partner, the surgical technique used, and the surgeon’s experience.
Reasons for Reversal
Changes in marital status, loss of a child, or a change in financial situation can lead to a desire for more children. A small percentage of men may experience chronic pain after a vasectomy, and reversal is sometimes considered as a means to alleviate this pain.
Financial Implications
Vasectomy reversal is typically more expensive than the initial vasectomy and is often not covered by insurance. The cost can range significantly, often between $5,000 and $15,000. For those considering reversal, weighing the cost against the desire and likelihood of achieving pregnancy is crucial. Consulting with a fertility specialist can provide valuable insights into the potential success and help in making an informed decision.
Vasectomy reversal represents a journey back from a decision once considered final. It’s a path marked by emotional, medical, and financial considerations. For those contemplating this route, a thorough understanding of the procedure, its success rates, and the associated costs is essential in making a choice that aligns with their current life goals and circumstances.
Conclusion
Vasectomy, as a significant and deeply personal choice in a man’s life, represents more than just a medical procedure; it’s a decision intertwined with one’s lifestyle, family planning goals, and long-term wellbeing. This exploration into the realms of vasectomy has underscored the procedure’s high success rate as a contraceptive method, its relative simplicity, and the profound considerations it entails.
From understanding the procedure and its permanent nature to evaluating the reasons men opt for vasectomy and the financial implications it carries, the journey is one that demands careful thought and informed decision-making. The possibility of reversal, while offering a potential path back, further highlights the need for certainty and clarity before proceeding with the original decision.
The role of healthcare professionals in this journey is indispensable. Thorough consultations, detailed discussions about the procedure, its effectiveness, potential complications, and post-procedure care are fundamental in ensuring that the decision to undergo a vasectomy is well informed and aligns with the individual’s life situation and future aspirations.