Hypertension during pregnancy
Pregnancy is a journey filled with joy and anticipation, but it also brings a host of medical concerns that require careful attention. One of the prime concerns is high blood pressure, a condition that can pose significant risks to both the mother and the developing baby. High blood pressure, or hypertension, during pregnancy is not just a common health issue; it is a complex one with various types and implications. This condition can manifest as chronic hypertension, gestational hypertension, or, in more severe cases, preeclampsia, each presenting its own set of challenges and risks.
Understanding high blood pressure during pregnancy is crucial for ensuring the short-term and long-term health and wellbeing of both mother and child. It is not just about managing a single health parameter; it is about comprehending a condition that intertwines with the intricate changes a woman’s body undergoes during these critical months. This blog aims to shed light on the nuances of high blood pressure in pregnancy, delving into its causes, types, potential complications, and management strategies. Through this exploration, we aspire to empower expectant mothers with knowledge, helping them navigate this aspect of pregnancy with confidence and informed vigilance.
1. What is high blood pressure in pregnancy?
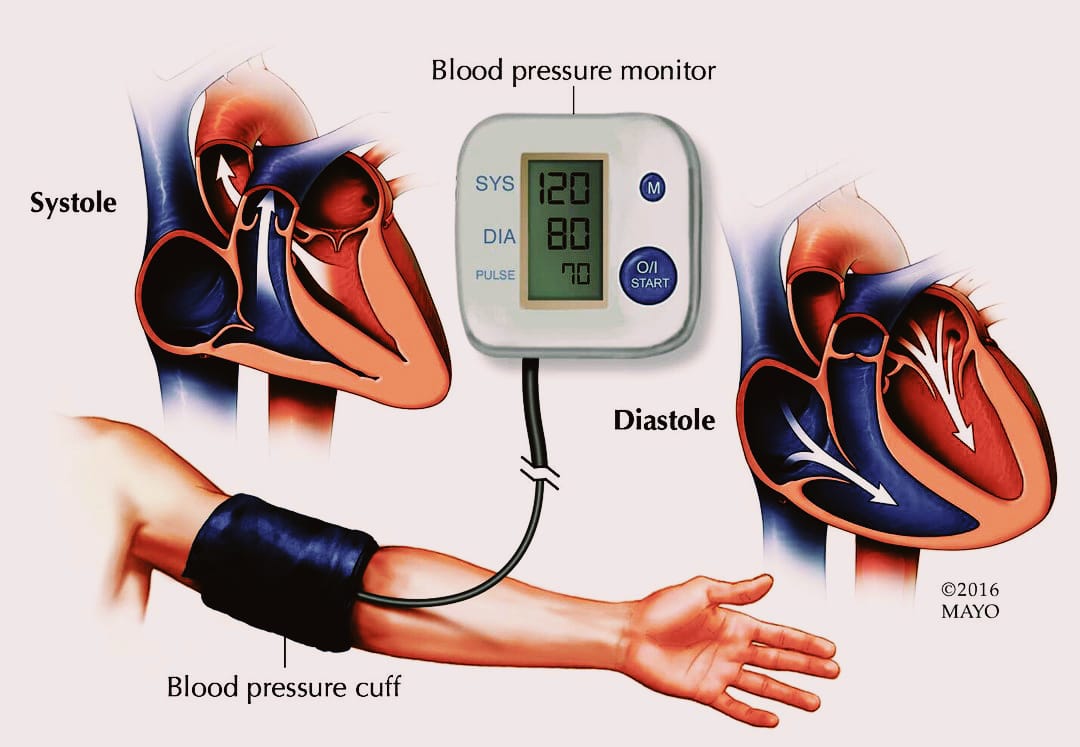
High blood pressure, or hypertension, is a condition where the force of the blood against the walls of the arteries is too high. In the context of pregnancy, this condition not only affects the mother’s health but also has significant implications for the developing fetus. Blood pressure is typically recorded with two numbers: the systolic pressure (the higher number) indicating the force your heart exerts on the walls of your arteries when it beats, and the diastolic pressure (the lower number) representing the pressure when your heart is at rest between beats. A normal blood pressure reading is around 120/80 mmHg, while higher readings indicate hypertension.
In pregnancy, hypertension is categorized into three primary types: chronic hypertension, gestational hypertension, and preeclampsia. Chronic hypertension is a symptom of high blood pressure that was present before pregnancy or that occurs before 20 weeks of gestation. Gestational hypertension, on the other hand, develops after the 20th week of pregnancy and usually resolves after childbirth. The most serious form is preeclampsia, a condition that develops after 20 weeks of gestation and is characterized not only by high blood pressure but also by signs of damage to other organ systems, most often the liver and kidneys.
The prevalence of these conditions varies, but they are a significant concern due to the risks they pose. Chronic and gestational hypertension can lead to complications such as decreased blood flow to the placenta, placental abruption, and preterm birth. Preeclampsia, if left unmanaged, can lead to multiple severe complications, including eclampsia, a serious condition that can cause seizures in the mother.
2. Causes and Risk Factors of High blood pressure
High blood pressure during pregnancy can be attributed to a variety of causes and risk factors, which vary depending on whether the condition is chronic or gestational. Chronic hypertension often predates pregnancy and may be due to underlying health conditions such as kidney disease, diabetes, or heart problems. In contrast, gestational hypertension develops specifically during pregnancy, and its exact cause is not completely understood, though it is believed to be related to how the placenta connects with the blood vessels in the uterus.
Several risk factors contribute to the likelihood of developing high blood pressure during pregnancy. Age plays a significant role; women over the age of 35 are at a higher risk. Lifestyle factors also have an impact—obesity, smoking, and a sedentary lifestyle can all increase the risk of hypertension. The medical history of the expectant mother is another crucial factor. A history of high blood pressure, kidney disease, or previous complications in pregnancy such as preeclampsia elevates the risk. Additionally, first-time mothers are more likely to develop gestational hypertension.
Genetic factors also play a role in the development of high blood pressure during pregnancy. Women with a family history of hypertension or preeclampsia are more prone to these conditions. Moreover, multiple gestations, such as twins or triplets, increase the risk of hypertension due to the additional strain on the body.
3. Complications and Risks
High blood pressure during pregnancy, if not properly managed, can lead to several complications that can affect both the mother and the baby. The risks associated with this condition make it a significant concern in prenatal care.
For the mother, chronic hypertension can increase the risk of developing more severe conditions like preeclampsia, a serious complication that can lead to organ damage and is characterized by protein in the urine. Preeclampsia, if it progresses to eclampsia, can cause seizures and is a major cause of maternal morbidity and mortality. Chronic hypertension also elevates the risk of cardiovascular diseases and kidney damage in the long term.
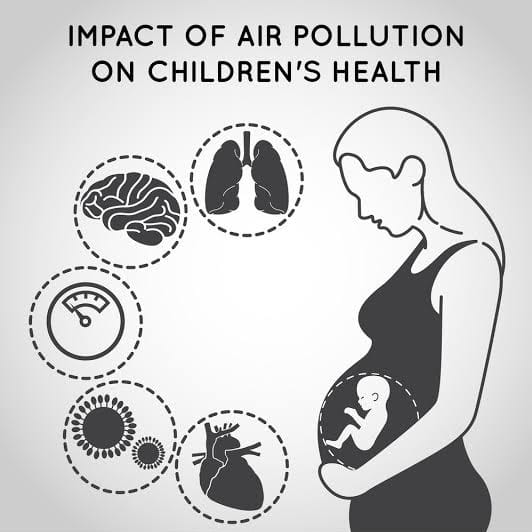
The baby’s health can also be impacted significantly. High blood pressure can lead to decreased blood flow to the placenta, which means less oxygen and nutrients for the baby. This can result in low birth weight, slowed growth (intrauterine growth restriction), and preterm birth, which is birth before 37 weeks of gestation. Preterm babies often face various challenges, including respiratory distress syndrome and other long-term health issues.
In cases of severe high blood pressure, there is a risk of placental abruption, a serious condition where the placenta separates from the inner wall of the uterus before delivery. This can lead to heavy bleeding and is a threat to both the mother and the baby. Furthermore, gestational hypertension can evolve into chronic hypertension post-pregnancy, with lasting effects on the mother’s health.
4. Diagnosis and Monitoring
The diagnosis and monitoring of high blood pressure during pregnancy are critical components of prenatal care. Blood pressure is typically measured at every prenatal visit using a standard blood pressure cuff. For a diagnosis of hypertension, blood pressure readings must be 140/90 mmHg or higher on two occasions, at least four hours apart. If a woman has chronic hypertension, this may be diagnosed before pregnancy or in the early stages, usually before 20 weeks of gestation. Gestational hypertension, however, is typically diagnosed after 20 weeks.
In addition to regular blood pressure measurements, healthcare providers may conduct further tests to monitor the health of both the mother and the fetus. These tests can include urine analysis to check for protein (a sign of preeclampsia), blood tests to assess kidney and liver function, and ultrasounds to monitor the baby’s growth and development. Doppler scans may also be used to examine blood flow in the placenta, ensuring the baby is receiving adequate nutrients and oxygen.
5. Management and Treatment
Effective management of high blood pressure during pregnancy involves a combination of lifestyle changes and, in some cases, medical treatment. The approach largely depends on the type of hypertension and its severity.
Lifestyle Changes includes
Diet: A healthy diet plays a crucial role in managing blood pressure. Expectant mothers are advised to eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Reducing salt intake is also key, as excessive salt can contribute to higher blood pressure.
Exercise: Regular, moderate exercise is beneficial. Activities like walking, swimming, and prenatal yoga can help maintain a healthy blood pressure level. However, it is important to consult with a healthcare provider before starting any exercise regimen during pregnancy.
Stress Management: Stress can be a contributing factor to high blood pressure. Techniques such as deep breathing, meditation, and prenatal massage can be effective in managing stress levels. Adequate rest and sleep are also important.
Medical Treatments:
In cases where lifestyle changes are not enough to control blood pressure, medication may be prescribed. It is essential that these medications are safe for use during pregnancy. Commonly prescribed drugs for hypertension in pregnancy include labetalol, nifedipine, and methyldopa. These medications have been shown to be safe for both the mother and the fetus when used under the guidance of a healthcare provider.
Regular monitoring of blood pressure and fetal health is an integral part of treatment. This may include more frequent prenatal visits and possibly additional ultrasound examinations.
Special Considerations:
In cases of preeclampsia, treatment may involve more aggressive interventions, including hospitalization and early delivery if necessary. The health of both the mother and baby is the priority, and decisions are made on a case-by-case basis.
6. Prevention Strategies
Preventing high blood pressure during pregnancy begins even before conception and continues throughout the pregnancy. Early planning and consistent prenatal care are crucial steps in this process.
Pre-Pregnancy Planning:
For those planning to conceive, a pre-pregnancy checkup is advisable. This can help identify and manage any existing health issues that might contribute to high blood pressure.
Achieving a healthy weight before pregnancy can also reduce the risk. Obesity is a known risk factor for hypertension, so a balanced diet and regular exercise are recommended to attain a healthy BMI.
Early and Regular Prenatal Care:
Once pregnant, early and regular prenatal visits are essential. These appointments allow healthcare providers to monitor blood pressure and catch any increases early.
Consistent prenatal care also provides the opportunity for education and guidance on maintaining a healthy pregnancy.
7. When to Seek Medical Help
It is crucial for pregnant women to be aware of symptoms that may indicate a need for immediate medical attention related to high blood pressure. These symptoms include severe headaches, changes in vision (such as blurred vision or seeing spots), sudden swelling of the face and hands, and upper abdominal pain, especially under the ribs on the right side. Experiencing shortness of breath or noticing a decrease in fetal movement are also warning signs that should not be ignored.
Prompt communication with healthcare providers is key when any of these symptoms occur. These signs could indicate preeclampsia or other serious complications related to high blood pressure, which require urgent medical intervention. Expectant mothers should never hesitate to contact their doctor or midwife if they experience any concerning symptoms, as early detection and treatment can be critical for the health and safety of both the mother and the baby
Navigating high blood pressure during pregnancy is a journey that requires awareness, vigilant management, and consistent prenatal care. From understanding the various types of hypertension, recognizing their causes and risk factors, to being aware of potential complications, this condition demands attention and understanding. Implementing lifestyle changes, adhering to medical treatments when necessary, and adopting preventive strategies are key components in managing this health challenge. Most importantly, recognizing the signs that necessitate immediate medical attention can be crucial for the safety of both mother and baby.