Pneumonia in babies
Pneumonia in newborns is a serious condition characterized by inflammation of the lungs, which can lead to difficulty breathing, reduced oxygen levels, and other complications. Due to their vulnerable immune systems and delicate physiology, newborns are particularly susceptible to respiratory infections. This article explores the causes, diagnosis, and management of pneumonia in newborns, providing a comprehensive overview for caregivers and healthcare professionals.
What is Pneumonia in Newborns?
Pneumonia is an infection of the lungs that causes inflammation and swelling. In newborns, pneumonia can be particularly challenging due to their underdeveloped immune systems and respiratory structures. The condition can be caused by a variety of pathogens, including bacteria, viruses, and fungi.
Causes of Pneumonia in Newborns
1. Bacterial Pneumonia
Group B Streptococcus (GBS): A common cause of early-onset pneumonia, usually acquired from the mother during delivery.
Escherichia coli (E. coli): Can also cause early-onset pneumonia, particularly in preterm infants.
Staphylococcus aureus: Including Methicillin-resistant Staphylococcus aureus (MRSA), which can lead to severe infections.
Klebsiella pneumoniae: May cause severe disease, particularly in neonates with underlying health issues.
2. Viral Pneumonia
Respiratory Syncytial Virus (RSV): A common cause of viral pneumonia in infants, leading to bronchiolitis and pneumonia.
Influenza Virus: Can also cause pneumonia, particularly during flu season.
Human Metapneumovirus (hMPV): Another virus that can cause respiratory infections in newborns.
3. Fungal Pneumonia
Candida Species: Can cause invasive fungal infections in very preterm or immunocompromised newborns.
Aspergillus Species: Rare but can occur in very high-risk infants or those with severe immune deficiencies.
4. Aspiration Pneumonia
Meconium Aspiration: Occurs when a newborn inhales a mixture of meconium (first stool) and amniotic fluid during or shortly after birth.
5. Nosocomial Pneumonia
Hospital-Acquired Infections: Infections acquired during hospitalization, particularly in very preterm or critically ill infants.
Diagnosis of Pneumonia in Newborns
1. Clinical Assessment
Diagnosis often begins with a clinical evaluation based on symptoms and physical examination:
Symptoms: Rapid or labored breathing, grunting, cyanosis (bluish skin), poor feeding, lethargy, or fever.
Physical Exam: Findings may include abnormal lung sounds (rales or wheezes), increased respiratory rate, and signs of respiratory distress.
2. Diagnostic Tests
Several tests may be used to confirm the diagnosis and identify the causative agent:
Chest X-Ray: To visualize lung abnormalities, such as infiltrates or consolidation.
Blood Tests: To assess for signs of infection, including white blood cell count, C-reactive protein (CRP), and blood cultures.
Sputum Culture: If possible, to identify bacterial or fungal pathogens.
Polymerase Chain Reaction (PCR): For detecting viral pathogens.
3. Prenatal Testing
For at-risk infants, prenatal testing and monitoring can help identify potential issues:
Maternal Screening: Testing for infections such as Group B Streptococcus in the mother during pregnancy.
Ultrasound: Monitoring for signs of fetal distress or meconium in the amniotic fluid.
Management and Treatment
1. Antibiotic Therapy
Bacterial Pneumonia: Treatment typically involves intravenous (IV) antibiotics, tailored to the specific pathogen identified or based on empirical guidelines.
Broad-Spectrum Antibiotics: Often used initially until specific pathogens are identified.
2. Antiviral and Antifungal Therapy
Viral Pneumonia: Supportive care is often the primary treatment, though antiviral medications may be used for specific viruses like influenza.
Fungal Pneumonia: Antifungal medications are used based on the specific fungal pathogen identified.
3. Supportive Care
Oxygen Therapy: To maintain adequate oxygen levels and relieve respiratory distress.
Ventilatory Support: In severe cases, mechanical ventilation or continuous positive airway pressure (CPAP) may be required.
Fluid Management: Ensuring adequate hydration and electrolyte balance, often through intravenous fluids.
4. Monitoring and Follow-Up
Continuous Monitoring: Vital signs, oxygen levels, and respiratory status should be continuously monitored.
Regular Assessments: Frequent evaluations to assess response to treatment and adjust care as needed.
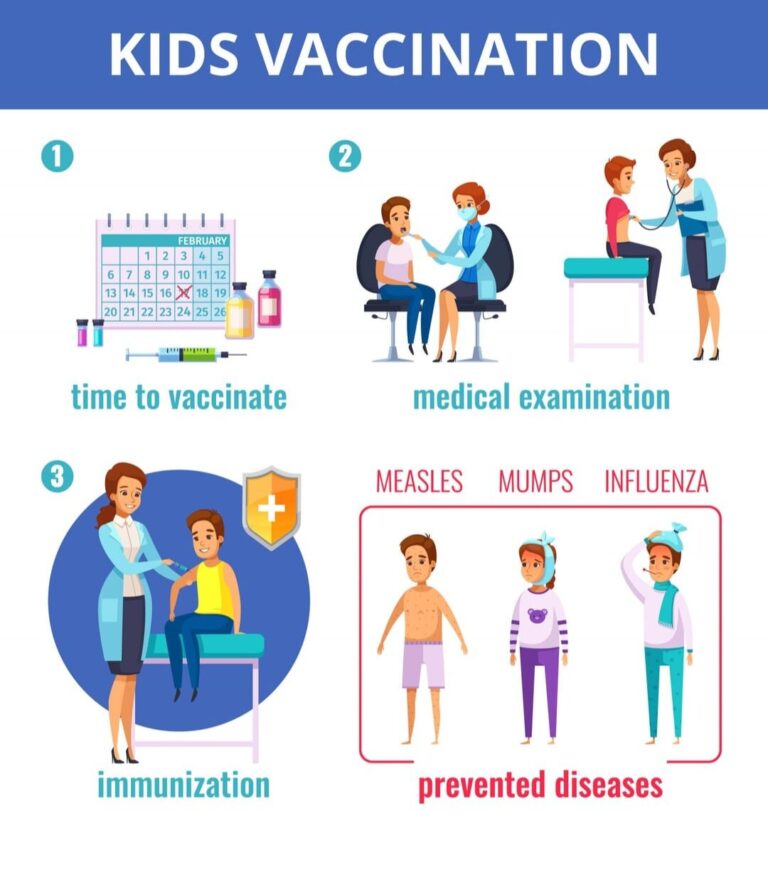
5. Preventive Measures
Maternal Screening and Treatment: Screening for and treating infections in pregnant women to reduce the risk of transmission.
Vaccination: Ensuring that both mothers and newborns receive appropriate vaccinations, such as the influenza vaccine.
Hand Hygiene: Strict handwashing protocols for healthcare workers and visitors to prevent the spread of infections.
Long-Term Outlook
The prognosis for newborns with pneumonia largely depends on the severity of the infection, the causative agent, and the overall health of the infant:
Full Recovery: Many newborns with pneumonia recover completely with appropriate treatment and supportive care.
Complications: Severe pneumonia can lead to complications such as lung damage, chronic respiratory issues, or developmental delays, especially in very preterm or critically ill infants.
Follow-Up: Regular follow-up appointments may be necessary to monitor recovery and address any long-term effects or complications.
Conclusion
Pneumonia in newborns is a serious condition that requires prompt diagnosis and treatment. Understanding the causes, recognizing the symptoms, and implementing effective management strategies are essential for improving outcomes and ensuring the health of affected infants. Through a combination of medical treatment, supportive care, and preventive measures, healthcare providers can effectively manage pneumonia and support the recovery of newborns.